How to Identify High-Alert Medications Requiring Double Checks in Clinical Settings

Every year, thousands of patients are harmed because a medication was given wrong-wrong dose, wrong patient, wrong route. Most of these errors happen with drugs that seem harmless on the surface but can kill if misused. These are called high-alert medications. They don’t cause more errors than other drugs, but when they do go wrong, the results are catastrophic. That’s why hospitals and clinics have strict rules around them: independent double checks. But not every high-alert drug needs the same level of scrutiny. Knowing which ones truly require two sets of eyes is critical-and it’s not as simple as checking every IV bag on the cart.
What Makes a Medication High-Alert?
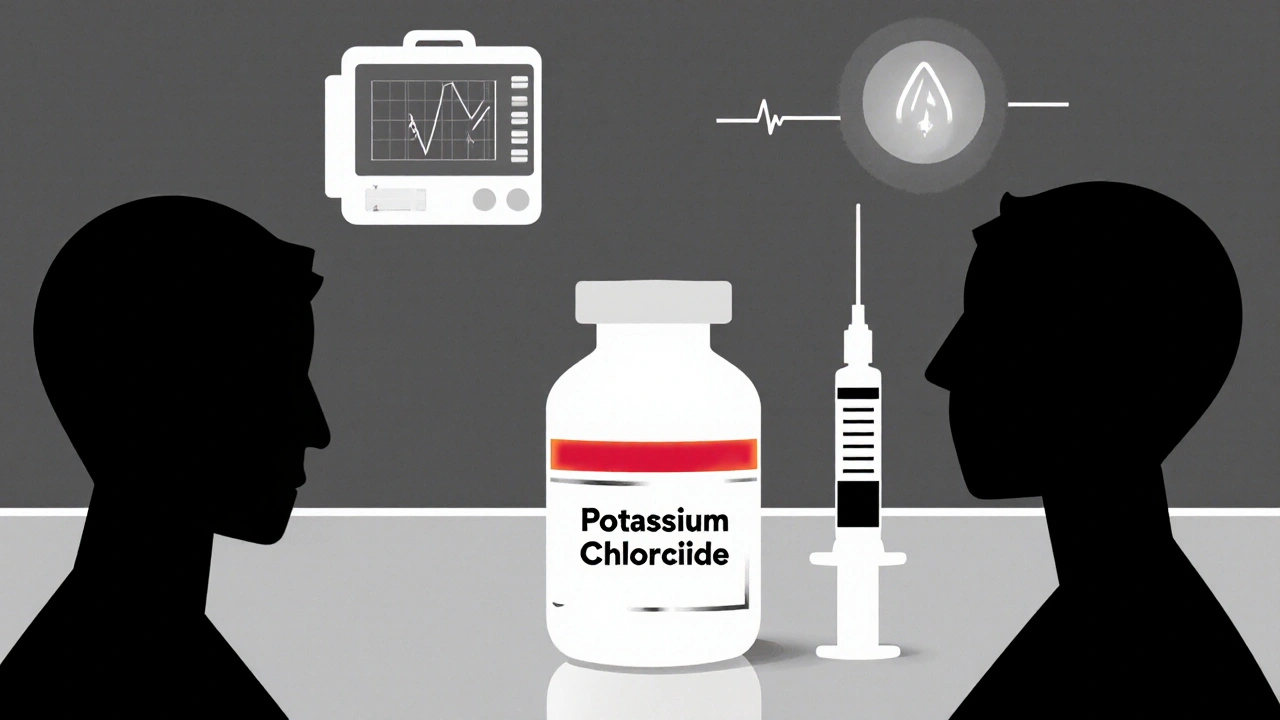
A high-alert medication isn’t defined by how often it’s used, but by how dangerous it is when something goes wrong. The Institute for Safe Medication Practices (ISMP) has been tracking these since 2001, and their latest list, updated in January 2024, includes 19 categories of drugs that demand extra safeguards. These aren’t just strong drugs-they’re drugs with a razor-thin margin between helping and harming.Take insulin, for example. A single wrong decimal point-giving 10 units instead of 1-can send a patient into a coma. Potassium chloride concentrate? One improperly diluted vial can stop a heart. Heparin infusions? Too much causes uncontrolled bleeding; too little lets clots form. These aren’t hypothetical risks. ECRI Institute reports that when double checks are done right, they stop 95% of these errors before the drug reaches the patient. But if the check is rushed, or if both staff members talk to each other while verifying, that number plummets to 40%.
So the question isn’t just: Which drugs are dangerous? It’s: Which ones are dangerous enough that human verification is still the best last line of defense?
Which Medications Absolutely Require a Double Check?
Not every high-alert drug needs a two-person check. Some are better protected by technology-smart pumps, barcode scanning, automated alerts. But for the highest-risk ones, human eyes are non-negotiable. Here’s what most major healthcare systems agree on:- IV insulin (both infusions and bolus pushes)
- Neuromuscular blocking agents (like succinylcholine or rocuronium)-used in intubation, but fatal if given to a conscious patient
- Potassium chloride concentrate (1 mEq/mL or higher)
- Potassium phosphate concentrate (1 mEq/mL or higher)
- IV heparin (including flushes over 100 units/mL)
- Chemotherapeutic agents (all forms, especially in pediatric oncology)
- Injectable narcotic PCA pumps (patient-controlled analgesia)
- Total parenteral nutrition (TPN) and lipid infusions
- Direct thrombin inhibitors (argatroban, bivalirudin)
- High-concentration sodium chloride (above 0.9%)
Some institutions, like Providence Health System, also require double checks for ketamine, CRRT solutions, and all controlled substances. Others, like the Veterans Health Administration (VHA), apply it universally to every drug on the ISMP list. But the trend is shifting. Experts now warn against blanket rules. The goal isn’t to check everything-it’s to check what matters most.
The Five Elements of a Proper Double Check
A double check isn’t just two people glancing at a label. It’s a structured, independent verification process. The VHA’s 2024 directive spells it out clearly: each clinician must verify five things-alone, without talking to the other person-before comparing notes.- Right patient - Two forms of ID: name and date of birth, scanned or spoken aloud. No room for assumptions.
- Right medication - Match the drug name on the label to the electronic order. Don’t assume “this looks like insulin”-confirm the name.
- Right dose - Calculate the dose yourself. Don’t trust the pharmacy label alone. If it’s a concentration like 100 units/mL heparin, verify the math.
- Right route - Is this meant for IV? Subcutaneous? Oral? Giving a concentrated potassium solution IV instead of PO is lethal.
- Right time - Is this dose due now? Or is it scheduled for later? Administering a dose early or late can cause dangerous fluctuations.
And here’s the critical part: they must do this separately. No standing side-by-side, no saying, “I think this is 5 units.” One person checks, writes down their findings, then walks away. The second person does the same. Only after both are done do they compare. If they disagree, they stop. No exceptions.
Why Most Double Checks Fail
You’ve probably seen it: two nurses standing at the bedside, one holding the medication, the other nodding along. They say “checked,” sign the eMAR, and move on. That’s not a double check. That’s a rubber stamp.A 2017 study in the Journal of Patient Safety found that when nurses performed “simultaneous checks”-meaning they did it together-the error detection rate dropped to 32%. Why? Because human brains are wired to confirm what they expect to see. If the first nurse says, “This looks right,” the second one subconsciously looks for reasons to agree, not reasons to question.
Another issue? Time. Nurses report adding 2-3 minutes per double check. In a busy unit, that’s hard to swallow. Some skip it. Others fake it. A 2023 Reddit thread from ICU nurses revealed a pattern: “I’ve caught three real errors in six months. But I’ve seen twelve checks where both people just signed without looking.”
And then there’s the chaos of emergencies. In the ER, during a code, there’s often no second nurse available. A 2021 survey of 850 emergency nurses found 82% said they couldn’t find a second person during critical resuscitations. So they bypass the check-or worse, they do it after the fact.
How to Make Double Checks Work
The best hospitals don’t just mandate double checks-they design systems around them.1. Train like it matters - Cleveland Clinic requires a two-hour competency module. Nurses must pass a simulation test where they catch a deliberately hidden error. 95% pass. Those who don’t get retrained.
2. Build time into the workflow - Mayo Clinic includes double-check time in staffing models. If you’re giving insulin, you’re not expected to rush. The system assumes you need those extra minutes.
3. Use technology as a partner, not a replacement - Smart pumps that block unsafe doses, eMAR systems that require dual electronic signatures, barcode scanners that flag mismatches-these reduce the burden. But they don’t eliminate the need for human verification. At 78% of Magnet-recognized hospitals, dual eMAR signatures are mandatory for high-alert meds.
4. Audit and give feedback - Johns Hopkins Hospital reduced heparin dosing errors from 12.7% to 2.3% in 18 months by auditing double checks and giving nurses real-time feedback. “We didn’t punish mistakes-we fixed the system,” one nurse said.

The Future: Less Manual, More Smart
The healthcare industry is moving away from blanket double checks. The ISMP now recommends using them only for the highest-risk scenarios: IV insulin, chemotherapy, and patients with complex conditions like renal failure.Technology is catching up. As of Q2 2024, 65% of large hospitals have smart pumps that communicate with eMAR systems. These can auto-calculate doses, flag concentration errors, and even lock out unsafe infusions. AI-assisted verification tools are in pilot at 12% of academic centers. In five years, manual double checks may drop by 40%.
But here’s the truth: technology can’t replace judgment. A pump can’t know if a patient’s kidney function changed overnight. A barcode can’t tell you if the patient is now on dialysis. That’s why, for now, the human eye still matters-especially when it’s truly independent.
What You Can Do Today
If you’re a clinician:- Know your institution’s list of high-alert medications. Ask if it’s aligned with ISMP’s 2024 list.
- Never do a double check with someone standing next to you. Walk away. Write it down. Then compare.
- If you’re pressured to skip a check, say so. Patient safety isn’t negotiable.
If you’re a manager:
- Don’t require double checks for every high-alert drug. Focus on the top 5-7 that cause the most harm.
- Invest in training-not just one-time lectures, but simulations and audits.
- Make sure your eMAR system requires dual signatures and blocks workarounds.
Medication safety isn’t about checking every box. It’s about checking the right ones-with care, independence, and purpose.
What are the most common high-alert medications that require a double check?
The most common high-alert medications requiring independent double checks include IV insulin, neuromuscular blocking agents, potassium chloride concentrate (1 mEq/mL or higher), IV heparin (including flushes over 100 units/mL), chemotherapy drugs, injectable narcotic PCA pumps, total parenteral nutrition (TPN), and high-concentration sodium chloride solutions. These are consistently flagged by ISMP, VHA, and major hospital systems due to their narrow therapeutic index and potential for rapid, life-threatening harm if dosed incorrectly.
Is a double check always required for every high-alert medication?
No. The Institute for Safe Medication Practices (ISMP) explicitly advises against universal double checks. Instead, they recommend a risk-based approach. For example, smart pumps with dose error reduction systems may be sufficient for some medications like certain anticoagulants. Double checks are reserved for the highest-risk scenarios-such as IV insulin in diabetic patients, pediatric chemotherapy, or concentrated electrolytes-where human judgment and verification are still the most reliable safety net.
What happens if the two people doing the double check disagree?
If the two clinicians disagree on any part of the verification-dose, route, patient ID, or timing-they must stop immediately. The medication should not be administered until the discrepancy is resolved. This may involve consulting a pharmacist, reviewing the original order, or checking the patient’s chart. No exceptions. This step is critical: the purpose of the double check is to catch errors, not to confirm assumptions.
Can a pharmacist do the second check instead of a nurse?
Yes, as long as the pharmacist is licensed and directly involved in the medication administration process. Many institutions allow pharmacists to serve as the second verifier, especially in settings like oncology units or ICUs where pharmacists are routinely present. The key requirement is independence-not the job title. The second person must verify without influence from the first and must be authorized to administer or verify the medication.
Why do some nurses resist doing double checks?
Many nurses resist because they feel it slows them down, especially during emergencies or when staffing is low. A 2022 survey found 63% of nurses reported difficulty finding a second person to verify. Others feel the process is performative-seen as a paperwork exercise rather than a safety tool. Resistance drops significantly when institutions provide training, protect time for checks, and show real results-like fewer errors and improved patient outcomes.
Are double checks required by law?
There is no federal law mandating double checks for all high-alert medications. However, The Joint Commission’s National Patient Safety Goal (NPSG.01.01.01), effective January 1, 2024, requires accredited organizations to identify high-alert medications and implement safeguards to prevent errors. Independent double checks are the most commonly accepted safeguard. Failure to implement appropriate safeguards can lead to accreditation issues and financial penalties under CMS Conditions of Participation.
How can technology improve the double-check process?
Technology enhances double checks by reducing human error and workload. Smart infusion pumps can auto-calculate safe dose ranges and block unsafe settings. eMAR systems require dual electronic signatures, creating an audit trail. Barcode scanning ensures the right patient, drug, and dose are matched. AI tools in pilot programs can flag discrepancies in real time. These don’t replace human verification-they make it more accurate and efficient, allowing staff to focus on complex decisions rather than routine checks.
Josh Gonzales
November 25, 2025 AT 23:46Been doing this for 12 years in ICU. The only thing that actually stops errors is the five-point verification. Not the checklist, not the barcode, not the smart pump. It’s the silence between the two people checking. No talking. No nodding. Just eyes on the label, the order, the patient ID. I’ve caught a 10x potassium dose because the second nurse didn’t say a word. She just wrote down 10 mEq and I wrote 100. We stopped. Saved a life. That’s it.
Valérie Siébert
November 26, 2025 AT 07:16YESSSS this is so real!!! I work in peds oncology and we do double checks on EVERY chemo dose like it’s a sacred ritual. And guess what? Last month I caught a nurse about to give vincristine IV instead of IT. She thought it was the same thing. We all freaked out. But the system WORKS. Stop treating it like a box to check and start treating it like your patient’s heartbeat.
Erika Hunt
November 27, 2025 AT 08:01I really appreciate how this post doesn’t just list drugs-it explains the *why* behind the protocol. I’ve seen so many units implement double checks as a compliance exercise, not a safety one. And then wonder why errors keep happening. It’s not about the number of checks-it’s about the quality of attention. When you treat it like a ritual, not a chore, people actually look. And when they look, they see things they didn’t expect. That’s the magic.
Jack Riley
November 27, 2025 AT 12:54Let’s be real: the whole double-check system is a placebo for institutional guilt. We know smart pumps and AI will replace this in 5 years. But hospitals cling to it because it makes them look responsible. Meanwhile, nurses are burnt out, rushed, and forced to perform theater. The real problem isn’t the check-it’s the system that forces you to fake it to survive. We don’t need more checks. We need fewer meds, better staffing, and less bureaucracy.
Jacqueline Aslet
November 28, 2025 AT 16:16It is, of course, a matter of epistemological humility. The human cognitive apparatus is inherently fallible, and to rely upon a binary verification protocol-however well-intentioned-is to mistake procedural rigor for epistemic certainty. One must interrogate not only the medication, but the ontological status of the verification itself. Is the second verifier truly independent, or merely a performative echo? The institutional apparatus, in its desire for control, has created a simulacrum of safety. We are not preventing errors-we are ritualizing denial.
Caroline Marchetta
November 29, 2025 AT 13:59Oh wow, I’m so moved. I just cried. This post? It’s like someone finally understood the silent scream of every nurse who’s had to verify potassium while their unit is down to one RN and three code blues. And yes, I’ve seen the rubber-stamp checks. I’ve seen the sighs. I’ve seen the eye rolls. But you know what? I still do it. Because one day, I’ll be the one who says ‘wait’-and someone’s child will live. And that’s enough.
Jennifer Griffith
November 30, 2025 AT 16:15so like… is potassium chloride really that dangerous? i mean, its just salt right? like, i eat it on my potatoes
Andrew Camacho
December 1, 2025 AT 04:03Let’s not pretend this is about safety. It’s about liability. Hospitals don’t care if you live or die-they care if you sue them. That’s why they make you do double checks. Not because they love you. Because they’re scared of the courtroom. And guess what? If you’re a nurse who refuses to fake it? You’re labeled ‘difficult.’ If you’re the one who catches the error? You get a coffee mug. That’s the system. Don’t be fooled.
Roscoe Howard
December 3, 2025 AT 03:36As an American healthcare professional, I must say that our protocols are far superior to those in Canada and Europe. In our system, double checks are mandatory, standardized, and enforced with precision. In other countries, they treat it like a suggestion. That’s why our mortality rates are lower. We don’t cut corners. We don’t compromise. We do it right-because we’re Americans.
katia dagenais
December 4, 2025 AT 10:43You know what’s worse than a bad double check? A nurse who thinks they’re doing one because they nodded at someone while reading the label out loud. That’s not safety. That’s performance art. I’ve seen nurses do this in front of cameras during safety audits. They’re not checking the medication-they’re checking the box for the inspector. And the worst part? The system rewards them for it. They get promoted. They get praised. Meanwhile, the patient who got the wrong dose? They’re discharged with a thank-you note and a bill. We’ve turned safety into a corporate KPI. And we’re all complicit.
Andrew McAfee
December 5, 2025 AT 06:46Just came from a hospital in Texas where they use AI to flag high-alert meds before they even hit the cart. It reads the order, cross-checks the patient’s labs, and auto-suggests safe doses. Nurse just confirms. No two-person ritual. No wasted time. And guess what? Error rate dropped 70%. Maybe it’s time we stop romanticizing the clipboard and start trusting the algorithm. Not because we’re lazy. Because we’re smarter now.