Polysomnography: What to Expect During a Sleep Study and How Results Are Interpreted

When you’re tired all the time but can’t figure out why, your doctor might suggest a polysomnography - a sleep study that records what’s really happening while you sleep. It’s not just about snoring or tossing and turning. This test catches things your eyes can’t see: pauses in breathing, abnormal brain activity, leg jerks, heart rhythm changes, and even when you enter REM sleep too early. It’s the most detailed way doctors diagnose sleep disorders, and it’s not as scary as it sounds.
What Happens During a Polysomnography?
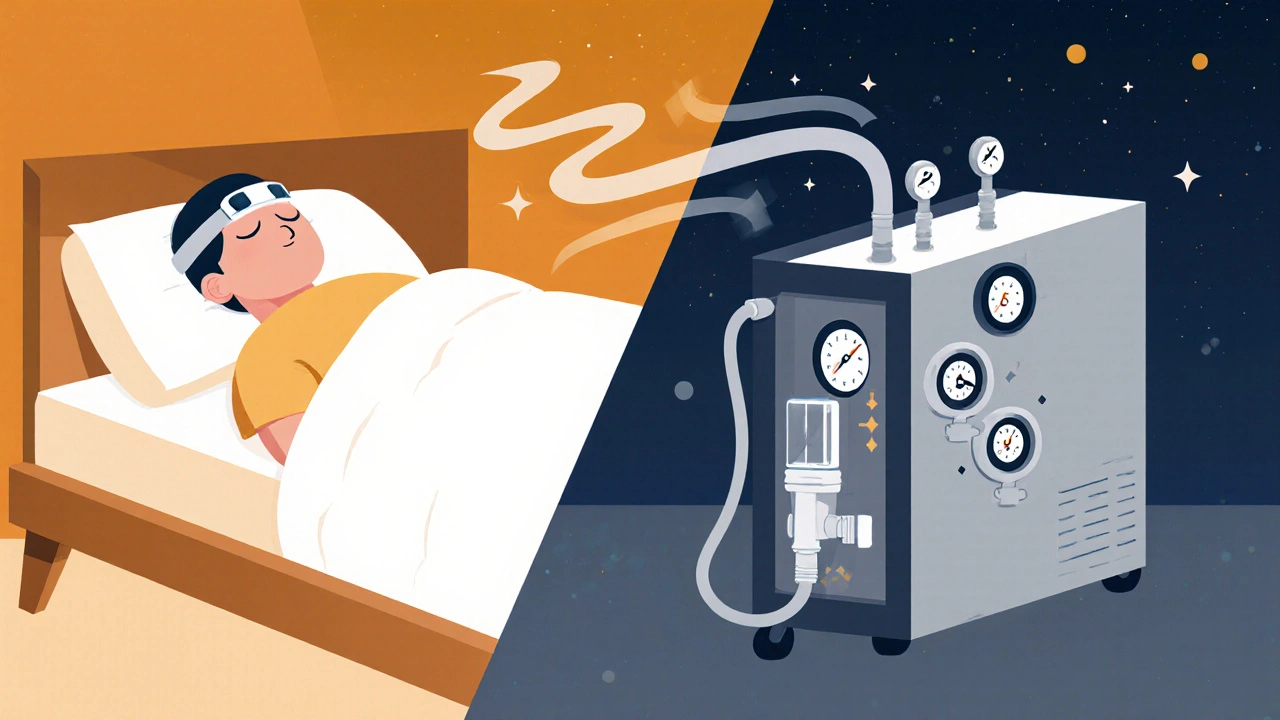
You’ll arrive at a sleep center in the evening, usually about an hour before your normal bedtime. The room looks like a hotel room - quiet, dim, with a comfortable bed. A sleep technologist will attach sensors to your scalp, face, chest, legs, and fingers. There are about 22 of them, but they’re small and lightweight. You won’t feel pain - just a little pressure or sticky residue from the electrodes.
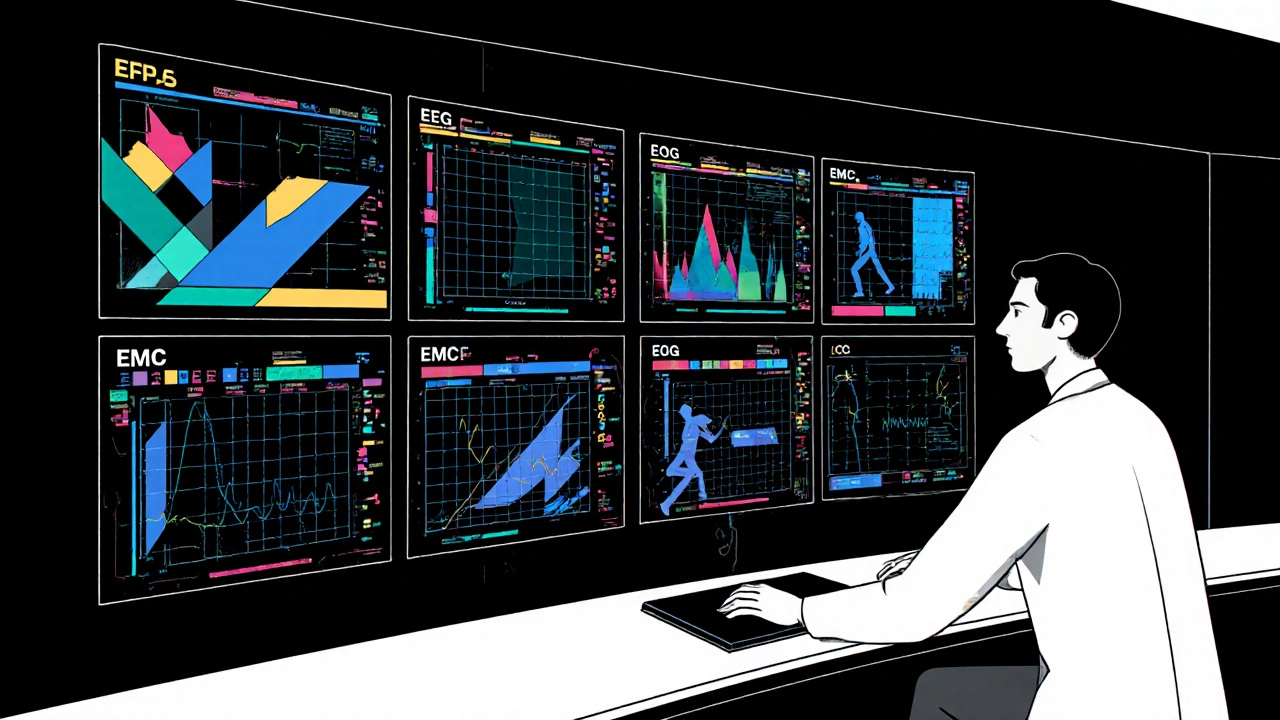
These sensors track seven key functions:
- Brain waves (EEG) - to see which sleep stage you’re in: light sleep, deep sleep, or REM.
- Eye movements (EOG) - to detect when you’re dreaming (REM sleep).
- Chin and leg muscle activity (EMG) - to catch restless legs or unusual movements.
- Heart rate and rhythm (ECG) - to spot irregular beats that happen only during sleep.
- Chest and belly movement - to tell if you’re trying to breathe even when air isn’t flowing.
- Airflow through nose and mouth - to detect if you’re stopping breathing.
- Blood oxygen levels - to see how much oxygen your body gets when you pause breathing.
A camera and microphone record sounds and movements too. You can talk to the tech anytime - if you need to use the bathroom, adjust your position, or just feel anxious. Most people sleep enough for a diagnosis, even if it takes a night or two to get used to the sensors.
Why Polysomnography Over Home Tests?
You might have heard about home sleep apnea tests. They’re cheaper and easier - just a small device you wear overnight at home. But they only measure three or four things: breathing effort, airflow, oxygen levels, and heart rate. That’s fine if your doctor is 95% sure you have obstructive sleep apnea.
But if you have other symptoms - like sudden muscle weakness during the day, acting out dreams, or unexplained daytime fatigue - a home test won’t cut it. Only a full polysomnography can catch:
- Narcolepsy - where you fall directly into REM sleep instead of going through normal sleep stages.
- REM sleep behavior disorder - when you physically act out dreams, sometimes violently.
- Central sleep apnea - where your brain stops sending the signal to breathe, unlike obstructive apnea where your airway collapses.
- Nocturnal seizures - confusing with parasomnias, but treated completely differently.
Home tests fail in 15-20% of cases because people don’t wear them right, or they miss key events. In-lab studies fail less than 5% of the time. Plus, if the tech sees you’re having apnea early in the night, they can start a CPAP titration right then - meaning you might leave with your treatment plan already set.
What Do the Results Show?
After your sleep study, a board-certified sleep doctor spends 2-3 hours analyzing over 1,000 pages of data. They don’t just look at how many times you stopped breathing. They check:
- How long you spent in each sleep stage - Do you get enough deep sleep? Did you enter REM too quickly?
- Apnea-hypopnea index (AHI) - The number of breathing pauses per hour. Over 5 is abnormal. Over 30 is severe.
- Oxygen drop frequency and depth - Did your blood oxygen fall below 90%? How often? How low did it go?
- Leg movements - More than 15 per hour can indicate restless legs syndrome.
- Heart rhythm changes - Did your heart skip beats or slow down too much during apneas?
- Body position - Do you breathe worse when lying on your back?
For example, if your AHI is 40 and your oxygen drops to 80% during sleep, you have severe obstructive sleep apnea. If your brain waves show you’re entering REM sleep within 5 minutes of falling asleep - instead of after 90 minutes - you might have narcolepsy. If your legs jerk every 20 seconds and you don’t remember it, you could have periodic limb movement disorder.
What If You Need CPAP?
If your study shows moderate to severe sleep apnea, the tech might switch you to a CPAP machine during the second half of the night. This is called a split-night study. It’s common - about 35% of polysomnography studies now include it.
The tech will gradually increase air pressure until your breathing pauses stop. By morning, they’ll know your ideal pressure setting. That means no second visit. You’ll get your machine and mask the same week. Many patients say this is the most helpful part - getting treatment the same night they get diagnosed.
How to Prepare for Your Sleep Study
Don’t change your routine. If you usually go to bed at 11 p.m., do that. If you nap during the day, skip it. Avoid caffeine after noon. No alcohol - it can mask sleep apnea. Don’t wear nail polish or lotions - they interfere with oxygen sensors.
Bring your own pillow, pajamas, and anything that helps you sleep. You can shower before bed. The sleep center will provide basic toiletries. Most people are surprised by how normal it feels - once the sensors are on, they forget they’re being monitored.
Who Covers the Cost?
Medicare covers 80% of polysomnography if you have documented symptoms like loud snoring, witnessed apneas, or excessive daytime sleepiness. Most private insurers require prior authorization. They’ll want your doctor to show you’ve tried lifestyle changes first - like losing weight or sleeping on your side.
Home tests cost 30-50% less, but if they’re inconclusive, you’ll still need an in-lab study. In the long run, getting the right diagnosis the first time saves money. Treating undiagnosed sleep apnea reduces risks of heart attack, stroke, and high blood pressure - costs that far outweigh the test.
Is It Worth It?
Over 90% of patients who get proper education before the test say they’d do it again. The discomfort is minor. The upside? Better sleep, more energy, clearer thinking, and fewer health risks. One patient told me, "I didn’t realize I was waking up 40 times a night - I thought I was just a light sleeper. After CPAP, I felt like I’d been asleep for a week straight."
Polysomnography isn’t perfect. Being in a lab can affect sleep for some. But it’s still the most complete picture we have of what happens when you’re unconscious. For complex cases, there’s no substitute.
Can I sleep normally with all those sensors?
Yes, most people do. While the first few minutes feel strange, the sensors are designed to be lightweight and non-restrictive. Sleep technologists are trained to help you relax - they’ll talk you through breathing exercises or adjust anything that feels uncomfortable. About 85% of patients get enough sleep for a valid diagnosis, even if it takes a little longer to fall asleep than usual.
Does polysomnography detect sleep apnea better than a home test?
Yes, for complex cases. Home tests only measure breathing and oxygen - they miss things like narcolepsy, leg movements, or central sleep apnea. Polysomnography tracks brain waves, eye movements, and muscle activity, giving a full picture of your sleep architecture. Home tests fail in 15-20% of cases; in-lab studies fail under 5%. If your symptoms are unclear, polysomnography is the only reliable option.
How long does it take to get results?
The study itself takes one night. But the analysis takes time - a sleep specialist reviews over 1,000 pages of data, which usually takes 2-3 hours. You’ll typically get your results within 7-10 business days. If you had a split-night study, your CPAP settings may be ready even sooner.
Can polysomnography diagnose narcolepsy?
Yes. Narcolepsy is diagnosed by measuring how quickly you enter REM sleep during the study. Normally, it takes 90 minutes to reach REM. People with narcolepsy enter REM within 15 minutes - sometimes even right after falling asleep. A second test, called the Multiple Sleep Latency Test (MSLT), is often done the next day to confirm the diagnosis.
Are there alternatives to in-lab polysomnography?
Home sleep apnea tests are the main alternative - but only for suspected obstructive sleep apnea with clear symptoms. For anything else - like unexplained fatigue, sleepwalking, or sudden muscle weakness - in-lab polysomnography is still the gold standard. Research is underway for simplified home versions, but none are as accurate or comprehensive yet.
What Comes Next?
If your results show a sleep disorder, your doctor will recommend treatment. For sleep apnea, that’s usually CPAP. For restless legs, it might be iron supplements or medication. Narcolepsy requires stimulants or sodium oxybate. REM behavior disorder often responds to clonazepam.
Follow-up is key. Many patients stop using CPAP after a few weeks because they don’t feel immediate results. But the benefits - better memory, lower blood pressure, less daytime sleepiness - build over months. If you’re struggling with your device, go back to your sleep center. There are dozens of mask types, pressure settings, and humidifiers to try.
Polysomnography doesn’t just find problems - it gives you back your life. If you’ve been tired for years, wondering why you can’t focus or why your partner says you stop breathing at night, this test is the first real step toward answers.
Amber O'Sullivan
November 11, 2025 AT 12:49Finally someone explains this without the medical jargon overload. I thought I was just a light sleeper until my wife recorded me stopping breathing 60 times in one night. The sensors felt weird at first but I slept better than I had in years. No regrets.
Lexi Brinkley
November 12, 2025 AT 05:55OMG YES!!! 😍 I did this last year and now I have a CPAP and I’m basically a new person. No more zombie mode at work. My boss asked if I got Botox or something lol. Sleep study = life upgrade 🙌
Kelsey Veg
November 14, 2025 AT 02:19lol so many ppl think home tests are good enough but they miss like 20% of stuff. i had a home test that said ‘normal’ then i went in lab and turned out i had central apnea plus narcolepsy. doc was like ‘you’re lucky u came in’ 🤯
Alex Harrison
November 14, 2025 AT 22:02I was skeptical too but the tech was super chill. They let me watch a movie before bed and gave me a warm blanket. The sensors didn’t hurt at all. I got diagnosed with PLMD and started iron supplements. My legs haven’t kicked like that in 10 years. Thanks for the info.
Jay Wallace
November 16, 2025 AT 13:21It’s amusing how people think home tests are ‘equivalent’-they’re not. Polysomnography is the gold standard for a reason. The fact that you need a board-certified sleep specialist to analyze 1,000 pages of data should tell you something. Home tests are for lazy people who don’t want to leave their couch. 😒
Alyssa Fisher
November 17, 2025 AT 04:46There’s something profound about being monitored while unconscious. It’s like your body is telling you secrets you’ve ignored for years. The data doesn’t lie. If you’re chronically tired, this isn’t about being lazy-it’s about biology screaming for attention. This test doesn’t just diagnose-it validates.
Alyssa Salazar
November 19, 2025 AT 00:24Let’s talk about REM latency. If you enter REM in under 15 minutes? That’s narcolepsy territory. Most docs don’t even check for it unless you’re falling asleep mid-conversation. My AHI was 48, oxygen dipped to 78%, and I didn’t even know I was stopping breathing. This isn’t ‘bad sleep’-it’s a neurological emergency.
Beth Banham
November 19, 2025 AT 16:12I was nervous about the whole thing but honestly? It was kind of peaceful. The room was quiet, the tech checked in gently, and I ended up sleeping more than I do at home. I think people fear it because they imagine it’s invasive. It’s really not. Just… observed.
Jim Oliver
November 19, 2025 AT 18:05Anyone who skips the in-lab study because it’s ‘inconvenient’ is just delaying their own health crisis. You think you’re saving money? You’re just buying a stroke later. And no, ‘I sleep fine’ doesn’t count. You’re not the judge of your own brain.
William Priest
November 20, 2025 AT 10:32CPAP titration in the same night? That’s not ‘convenient’-that’s the only ethical way to do it. Why make someone come back? Lazy clinics do home tests because they’re cheaper, not better. Real medicine doesn’t cut corners. This post is right-this is the gold standard. Period.
Ryan Masuga
November 21, 2025 AT 12:08Just want to say-this is one of the most helpful breakdowns I’ve seen. If you’re on the fence, DO IT. I was scared too. But waking up feeling like I’d slept 8 hours instead of 4? Worth every second. And yeah, the mask takes getting used to-but so does being exhausted all the time.
Jennifer Bedrosian
November 23, 2025 AT 01:04I cried after my results. Not because I had sleep apnea-but because I finally knew why I’d felt like a ghost for 12 years. My husband thought I was just ‘moody’. Turns out I was dying slowly from lack of oxygen. This test didn’t just fix my sleep-it saved my marriage.