ADHD Stimulants and MAOIs: Understanding the Risk of Hypertensive Crisis
MAOI to Stimulant Washout Period Calculator
Medication Transition Calculator
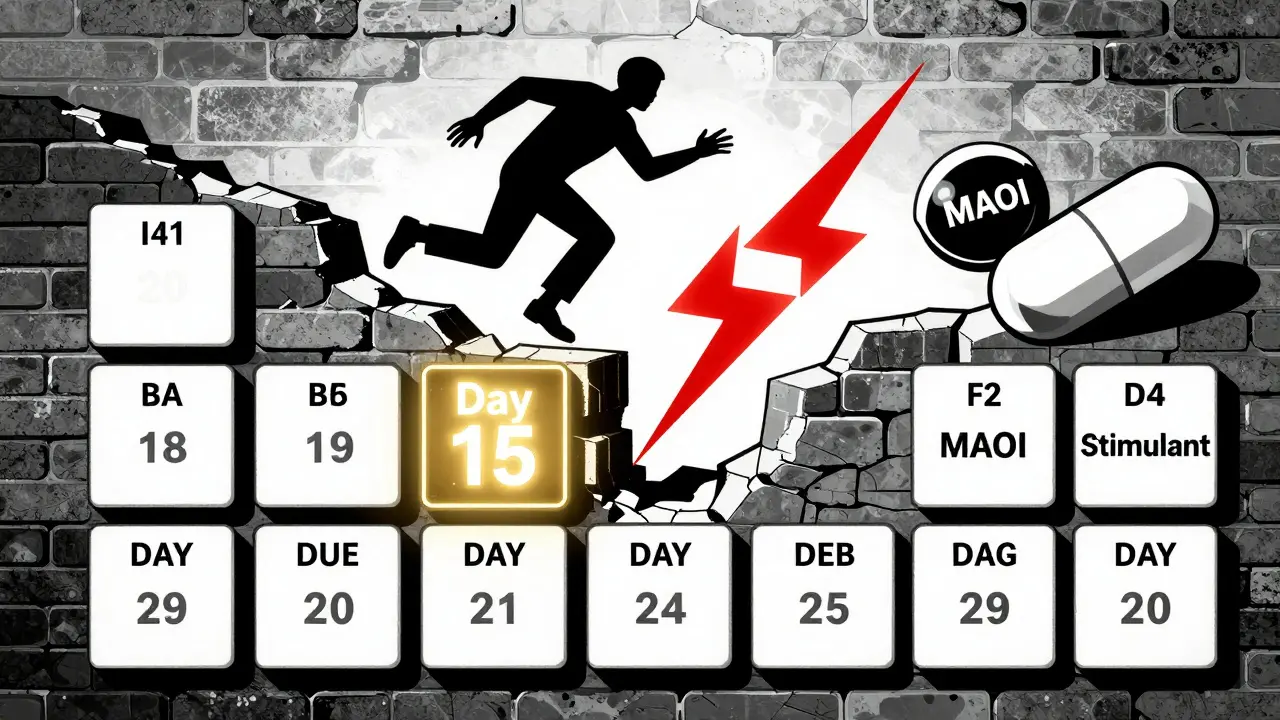
This calculator determines when it's safe to transition from MAOIs to ADHD stimulants or vice versa. The FDA requires a minimum 14-day washout period to allow your body to regenerate monoamine oxidase enzymes. Starting stimulants too soon can cause a dangerous hypertensive crisis.
Why This Matters
MAOIs bind permanently to monoamine oxidase enzymes. It takes 14 days for your body to produce enough new enzymes to safely handle stimulants again. Starting stimulants too soon can cause blood pressure to spike to dangerous levels (systolic >180 mmHg), potentially leading to stroke, heart attack, or brain hemorrhage.
Remember: This calculator shows when it's biologically safe to transition. It does NOT replace medical supervision. Your doctor will consider additional factors like your health history, other medications, and the specific drugs you're taking.
Combining ADHD stimulants with MAOIs isn't just a bad idea-it can be life-threatening. Even if you’ve been told this combination is "rare," the risks aren’t theoretical. People have died from it. Blood pressure can spike to dangerous levels within hours, leading to stroke, heart attack, or brain hemorrhage. This isn’t a "maybe"-it’s a hard stop unless you’re under the strict supervision of a specialist who knows exactly what they’re doing.
Why This Combination Is So Dangerous
ADHD stimulants like Adderall, Vyvanse, and Ritalin work by boosting dopamine and norepinephrine in the brain. That’s how they help with focus and impulse control. But norepinephrine also tightens blood vessels and raises heart rate. MAOIs-medications like phenelzine, tranylcypromine, and selegiline-are antidepressants that stop your body from breaking down those same chemicals. When you put them together, your body can’t clear the excess norepinephrine. It builds up. Fast.That’s when your blood pressure goes off the charts. Systolic readings above 180 mmHg and diastolic above 110 mmHg aren’t just "high"-they’re a medical emergency. The FDA’s own labeling for stimulants like APTENSIO XR says this combo can cause death, stroke, or aortic dissection. This isn’t a footnote. It’s a black box warning-the strongest kind.
Not All MAOIs Are the Same
You might hear that "some MAOIs are safer." That’s partially true, but it’s misleading. Older MAOIs like tranylcypromine and phenelzine block both MAO-A and MAO-B enzymes. That means they interfere with tyramine (a chemical in aged cheese, cured meats, and tap beer) and norepinephrine. Even small amounts of tyramine can trigger a sudden spike in blood pressure when you’re on these drugs.Transdermal selegiline (Emsam patch) is different. At low doses (6 mg/24h), it mostly targets MAO-B in the skin, not the gut. That means it doesn’t interfere with tyramine as much. The FDA even says dietary restrictions aren’t required at this dose. But here’s the catch: even this "safer" version still interacts with stimulants. The risk is lower, but it’s not gone. A 2023 clinical trial tracking 25 patients on low-dose selegiline and lisdexamfetamine reported no hypertensive crises-but that’s 25 people. We don’t know how it plays out in 10,000.
Stimulants Vary Too
Not all ADHD meds carry the same risk. Amphetamines-like Adderall and Vyvanse-are stronger at releasing norepinephrine than methylphenidate-based drugs like Ritalin or Focalin. A 2005 review found amphetamines cause more pronounced adrenergic effects. That means if you’re on an MAOI, amphetamines are riskier than methylphenidate.Even small doses matter. One case report from Cleveland Clinic described a 42-year-old patient who developed a systolic blood pressure of 210 mmHg after combining tranylcypromine with dextroamphetamine and psilocybin. That’s not an outlier. It’s a warning. The body doesn’t distinguish between "medical" and "recreational" stimulants when it comes to norepinephrine overload.
What About the "Rare" Cases?
You might read online that some doctors "do this safely." There are case reports-like one from Massachusetts General Hospital in 2017-where 12 patients were given lisdexamfetamine while on MAOIs, with no hypertensive events. But here’s what those reports don’t say: every single patient was monitored hourly for the first 24 hours. Their blood pressure was checked every 15 minutes during dose increases. They started at 10% of the normal dose. They avoided all tyramine-rich foods. They had no history of high blood pressure or heart disease.That’s not "common practice." That’s a highly controlled, resource-intensive protocol you won’t find at a regular clinic. Dr. Richard Friedman from Weill Cornell says he’s seen 200 cases without incident-but he’s a professor at a top academic hospital with access to 24/7 monitoring and emergency protocols. Most patients don’t have that.

The Washout Period Isn’t Optional
If you’re switching from an MAOI to a stimulant-or vice versa-you need to wait at least 14 days. Why? Because MAOIs bind permanently to the enzyme. Your body can’t make new ones overnight. It takes two weeks for your liver to produce enough fresh monoamine oxidase to safely handle stimulants again.Some people try to cheat this. They stop their MAOI on a Friday and start Adderall on Monday. That’s not safe. The enzyme doesn’t magically come back. The FDA’s guidelines are clear: no stimulants within 14 days of stopping an MAOI. And if you’re going off a stimulant to start an MAOI? Same rule applies. Wait two weeks.
Who Should Never Try This?
Even if you’re in a specialized clinic, you shouldn’t combine these drugs if you have:- Uncontrolled high blood pressure
- Heart disease, including arrhythmias or prior heart attack
- History of stroke or aneurysm
- Liver disease (MAOIs are processed by the liver)
- Any other medication that increases serotonin (SSRIs, SNRIs, tramadol, dextromethorphan)
Serotonin syndrome can happen too-another deadly combo. You don’t want to risk both hypertensive crisis and serotonin syndrome at the same time.
What to Do If You’re Already on Both
If you’re currently taking an MAOI and an ADHD stimulant, don’t panic-but don’t ignore it either. Stop the stimulant immediately and contact your prescriber. Don’t quit the MAOI cold turkey either. Abruptly stopping an MAOI can cause withdrawal symptoms like dizziness, nausea, or worsening depression.Work with your doctor to create a safe plan. That might mean switching your antidepressant to something like bupropion (Wellbutrin), which doesn’t interact with stimulants. Or, if your ADHD symptoms are severe and your depression is treatment-resistant, you might need to be referred to a specialist who can monitor you closely during a carefully timed transition.
What’s Changing in 2026?
MAOI use has dropped from 5% of antidepressant prescriptions in 2000 to less than 1% today. That’s because safer alternatives like SSRIs and SNRIs became available. But ADHD prescriptions have exploded-92 million in 2022 alone. That means more people are on stimulants, and more might end up needing an MAOI for depression that didn’t respond to other drugs.Research is ongoing. A 2023 trial (NCT04567891) is testing low-dose selegiline patch with lisdexamfetamine in 50 patients. Early results are promising, but it’s still early. The FDA hasn’t changed its stance. The black box warning remains. Until large-scale studies prove safety, the safest choice is still to avoid the combination.
Bottom Line: Don’t Risk It
This isn’t about being "overcautious." It’s about survival. The data is clear: combining ADHD stimulants and MAOIs can kill. Even if you’re young, healthy, and feel fine, your body doesn’t always show warning signs until it’s too late. Blood pressure spikes can happen without symptoms-until you collapse.If you’re on an MAOI, tell every doctor you see that you’re taking one. Don’t assume they know. If you’re on a stimulant, tell your psychiatrist if you’ve ever taken an MAOI-even if it was years ago. Write it down. Bring a list. Ask: "Is this safe with my current meds?"
There are other ways to treat treatment-resistant depression and ADHD together. Bupropion, atomoxetine, and even non-drug therapies like CBT or TMS can work. You don’t need to risk your life for a faster fix.
Can I take Adderall if I used an MAOI a year ago?
Yes. After a full 14-day washout period, the enzyme regenerates completely. A year is more than enough time. The 14-day rule is based on how long it takes your body to make new monoamine oxidase enzymes. Once that’s done, there’s no lingering risk. Just make sure you’re not still taking any MAOI, even in a different form.
Is it safe to take Vyvanse and the Emsam patch together?
Not without strict medical supervision. Even though the Emsam patch at 6 mg/24h has lower dietary risks, it still inhibits MAO enzymes enough to interact with Vyvanse. There’s no FDA approval for this combo. Only a specialist in a monitored setting should consider it, and even then, only after trying all other options. Start with a very low dose of Vyvanse and check blood pressure every 15 minutes for the first 24 hours.
What happens if I accidentally take both?
Call 911 or go to the nearest emergency room immediately. Don’t wait for symptoms. Hypertensive crisis can develop rapidly. Symptoms include severe headache, blurred vision, chest pain, nausea, or confusion. But sometimes, there are no warning signs until your blood pressure hits a critical level. Emergency treatment involves IV medications to lower blood pressure fast and monitoring for organ damage.
Can I drink alcohol while on an MAOI and an ADHD stimulant?
No. Alcohol can worsen the blood pressure effects of both drugs. It can also lower your blood pressure temporarily, then cause a rebound spike. That’s dangerous when combined with MAOIs and stimulants. Plus, alcohol can interact with MAOIs to cause dangerous spikes in tyramine levels. Avoid alcohol completely if you’re on either drug, and especially if you’re on both.
Are there any safe alternatives to MAOIs for depression if I need an ADHD stimulant?
Yes. Bupropion (Wellbutrin) is the most common alternative. It doesn’t interfere with MAO enzymes and works well with stimulants. Atomoxetine (Strattera) is a non-stimulant ADHD medication that can be combined with SSRIs or SNRIs. For treatment-resistant depression, options like ketamine infusions or transcranial magnetic stimulation (TMS) are increasingly used and don’t interact with stimulants. Talk to your doctor about these options before considering risky combos.
Next Steps If You’re Considering This Combo
If you’re thinking about combining these medications, here’s what to do:- Stop any self-researching online. Most of it is incomplete or misleading.
- Write down every medication, supplement, and over-the-counter drug you take.
- Ask your psychiatrist for a referral to a psychopharmacologist-a specialist who focuses on complex drug interactions.
- Get a home blood pressure monitor. Check it daily, especially in the morning and evening.
- Keep a log of symptoms: headaches, dizziness, chest tightness, blurred vision.
- Never start or stop either drug without medical guidance.
The goal isn’t to scare you. It’s to make sure you know the real stakes. There are safer paths. You don’t need to gamble your life for a quicker fix.
gary ysturiz
January 13, 2026 AT 09:48Just want to say this post saved my life. I was considering mixing Vyvanse with my MAOI because I thought "it’s just one time". Now I know better. Thanks for laying it out so clearly.
Jessica Bnouzalim
January 13, 2026 AT 20:20OMG, YES!! I’ve been on Emsam for 3 years and my psych just prescribed me Adderall last month-I panicked and called my doctor right away. They switched me to Wellbutrin and I feel better than ever. Don’t mess with this stuff!!
laura manning
January 14, 2026 AT 06:58It is imperative to note that the pharmacokinetic interaction between monoamine oxidase inhibitors and amphetamine derivatives is not merely theoretical; it is empirically documented in peer-reviewed literature, including the FDA’s black box warnings and clinical case reports from institutions such as Massachusetts General Hospital and the Cleveland Clinic. The risk of hypertensive crisis is neither negligible nor anecdotal-it is a well-characterized, life-threatening pharmacological phenomenon.
Bryan Wolfe
January 15, 2026 AT 22:58Hey, I get it-you’re tired of feeling depressed and sluggish. I’ve been there. But please, don’t risk it. I switched from an MAOI to Wellbutrin and added Strattera for my ADHD-and it’s been a game-changer. No crises, no scary BP spikes, just steady focus and calm. You don’t need to burn the bridge to get to the other side. There’s a safer path, and it’s worth waiting for.
Lauren Warner
January 17, 2026 AT 01:10People who say "I did it and lived" are either lying or incredibly lucky. You’re not a statistic-you’re a patient. And if you’re gambling with your life because you’re too impatient to wait 14 days, you’re not brave-you’re reckless. This isn’t a Reddit myth. It’s a death sentence waiting to happen.
Craig Wright
January 17, 2026 AT 02:14In the United Kingdom, such combinations are strictly prohibited under MHRA guidelines. The notion that "some doctors do it safely" is a dangerous American exceptionalism. We do not gamble with public health. The FDA warning exists for a reason. If you are considering this, you are not a pioneer-you are a liability.
Ben Kono
January 17, 2026 AT 20:56So if I took an MAOI a year ago I’m good right I mean like the enzyme is back right I’m not gonna die
Cassie Widders
January 19, 2026 AT 18:38My dad had a stroke from this combo back in 2010. He didn’t even know it was dangerous. I read this whole thing and cried. Please, if you’re reading this and thinking "it won’t happen to me"-it already happened to someone’s dad. Don’t be the next story.