Alcohol Types and Medication Safety: What You Need to Know About Spirits, Wine, and Beer
Alcohol-Medication Interaction Checker
Check Your Alcohol-Medication Risk
Enter your medication and alcohol type to see the risk level. Based on CDC and FDA guidelines.
More than 40% of adults take prescription medications while drinking alcohol - and most have no idea how dangerous that can be. It doesn’t matter if you’re sipping a glass of wine with dinner, knocking back a beer after work, or having a shot of whiskey before bed. The risk isn’t about the drink - it’s about the alcohol inside it. And when that alcohol meets your meds, things can go wrong fast.
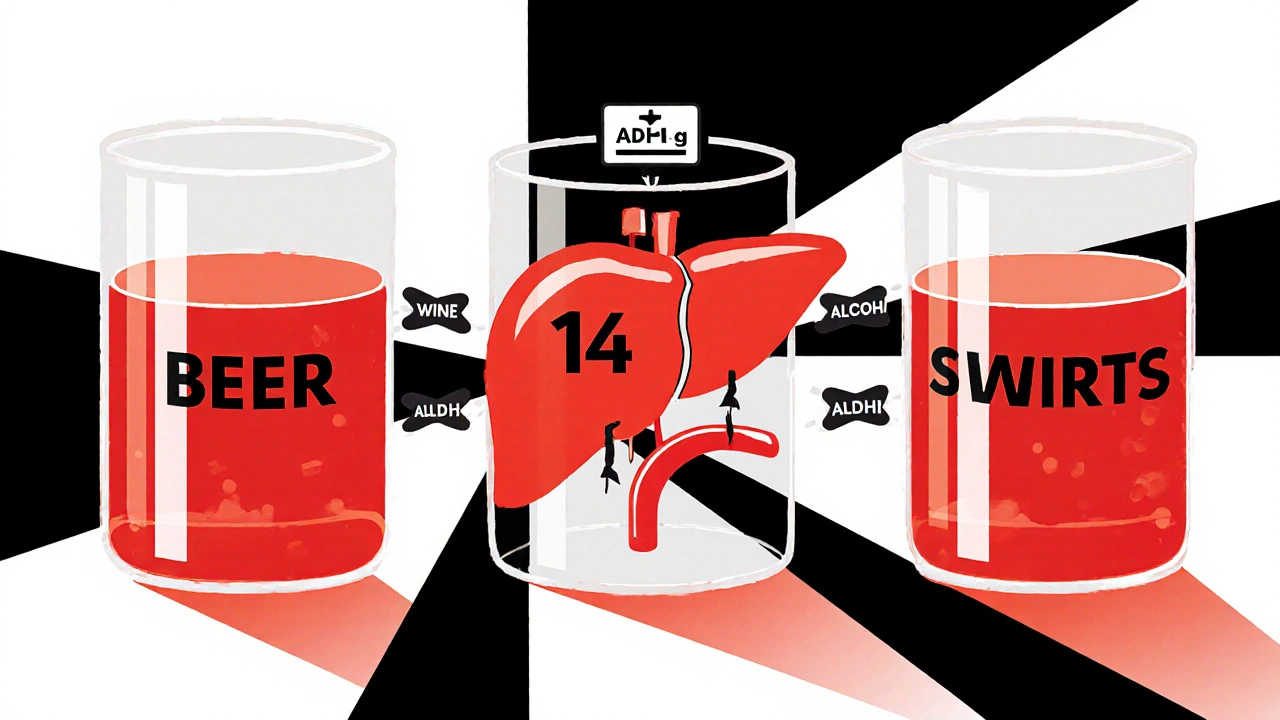
It’s Not the Drink, It’s the Alcohol
People often think red wine is safer than vodka, or that beer won’t hurt as much because it’s "light." That’s a myth. A standard drink - whether it’s 12 ounces of beer, 5 ounces of wine, or 1.5 ounces of spirits - contains the same amount of pure alcohol: 14 grams. That’s the key number. Your liver doesn’t care if the alcohol came from a pint of lager or a shot of gin. It processes it the same way.The liver uses enzymes like alcohol dehydrogenase (ADH) and aldehyde dehydrogenase (ALDH) to break down alcohol. But those same enzymes also handle dozens of common medications - including painkillers, antidepressants, antibiotics, and sleep aids. When alcohol and meds compete for the same enzymes, one or both can build up in your system. That’s when side effects get dangerous.
Spirits: Fast, Strong, and Riskiest
Spirits like whiskey, vodka, and rum pack the most punch in the smallest volume. One shot equals the alcohol in a whole can of beer. And because they’re usually consumed quickly - especially in social settings - your blood alcohol level spikes fast. That rapid rise is the problem.Emergency room data shows that 68% of alcohol-medication overdose cases involve spirits. Why? Because people think, "I only had one shot." But one shot of 40% alcohol hits your bloodstream harder and faster than a slow-drinking beer. Clinical trials show that when ethanol is absorbed quickly - like with spirits - interactions with benzodiazepines (like Xanax or Valium) become 40% more severe than when the same amount is sipped slowly.
That means if you take a sleep med and then have a shot of tequila, you could wake up groggy, confused, or even unresponsive. The next-day impairment isn’t just "feeling off" - it’s a real safety risk. One Reddit user shared: "Had one shot with my sleeping pill. Woke up at 3 a.m. unable to move. Thought I was having a stroke."
Wine: The "Healthy" Myth
Wine gets a bad rap for being unhealthy, but many people believe it’s the "safest" alcohol with meds. That’s dangerous thinking. Red wine contains polyphenols and tannins - plant compounds that can interfere with blood thinners like warfarin. One Mayo Clinic study found that red wine increased bleeding risk by 15% compared to the same amount of alcohol from spirits.And then there’s metronidazole - a common antibiotic. Mixing it with any alcohol can trigger a disulfiram-like reaction: flushing, pounding heart, nausea, vomiting, and even low blood pressure. But wine is the most commonly reported offender in user forums. Why? Because people think, "It’s just a glass of wine," and don’t realize even a small amount can trigger this reaction. One user wrote: "I had two sips of wine with my antibiotic. Felt like I was going to die."
The myth that red wine is "heart-healthy" and therefore safe with meds is misleading. No amount of polyphenols cancels out the risk when alcohol and meds are mixed.
Beer: The Silent Danger
Beer seems harmless because it’s low in alcohol - usually 4% to 7%. But here’s the catch: people drink it in volume. One beer? Fine. Four beers? That’s four standard drinks. And most people don’t count that way.CDC data shows beer accounts for 52% of total alcohol consumed in the U.S. - and 47% of unintentional alcohol-medication interactions happen because of beer. Why? Because people think, "I’m not drunk, I just had a few beers." But if you’re taking ibuprofen, those beers can cause stomach bleeding. If you’re on statins, they can raise your liver enzyme levels. If you’re on antidepressants, they can make you feel worse, not better.
One GoodRx user review said: "Took ibuprofen for my back pain. Had three beers. Woke up with black, tarry stools. ER said I almost bled out." That’s not rare. It’s predictable.

What About Non-Alcoholic Beer?
"Non-alcoholic" beer still contains up to 0.5% alcohol. That’s not enough to get you drunk - but it’s enough to interfere with certain medications. If you’re on metronidazole, disulfiram, or some seizure meds, even that tiny amount can cause a reaction. And if you’re taking a medication that’s processed by the liver, that 0.5% still adds up over time.Only 18% of adults know this. Most assume "non-alcoholic" means "safe." It doesn’t. Always check with your pharmacist - especially if you’re on long-term meds.
What Medications Are Most Dangerous With Alcohol?
Some meds are fine with occasional alcohol. Others? Never mix. Here’s the short list of high-risk combinations:- Benzodiazepines (Xanax, Valium, Ativan): Can cause extreme drowsiness, slowed breathing, coma, or death.
- Opioids (oxycodone, hydrocodone, morphine): Alcohol multiplies the risk of respiratory failure.
- Antidepressants (SSRIs, SNRIs): Can increase dizziness, drowsiness, and liver damage.
- Antibiotics (metronidazole, tinidazole, linezolid): Trigger severe reactions like flushing, nausea, and rapid heartbeat.
- Acetaminophen (Tylenol): Just two drinks can raise liver damage risk by 300% - even if you’re not a heavy drinker.
- Blood thinners (warfarin): Alcohol can make your blood too thin or too thick, depending on how much you drink.
- Diabetes meds (insulin, metformin): Alcohol can cause dangerously low blood sugar.
If your prescription label says "avoid alcohol," don’t assume it’s just a suggestion. It’s a warning.
How to Stay Safe
You don’t have to quit alcohol forever. But you do need to be smart:- Know your standard drink. 12 oz beer = 5 oz wine = 1.5 oz spirits. That’s it.
- Check every new med. Ask your pharmacist: "Is it safe with alcohol?" Don’t assume it’s fine.
- Don’t drink on an empty stomach. Food slows alcohol absorption. That gives your liver more time to process it.
- Avoid carbonated drinks. Champagne, soda mixes, and sparkling beers empty from your stomach faster - meaning alcohol hits your blood quicker.
- Use a free app. GoodRx’s "Alcohol Check" tool lets you enter your med and drink type to get a real-time risk alert.
- When in doubt, skip it. If you’re on a high-risk med, don’t risk it. One drink isn’t worth a hospital visit.
What’s Changing in 2025?
Hospitals and pharmacies are finally catching up. In 2023, the FDA approved a new system that generates alcohol interaction warnings based on beverage type - not just "alcohol." Starting in 2024, Medicare Part D requires pharmacists to give specific counseling for 27 high-risk meds, including exact guidance on spirits, wine, and beer.Electronic health records like Epic now flag alcohol-medication risks at the point of prescribing. One study showed this cut adverse events by 34% in just one year.
But technology can’t replace education. The NIH found that without visual aids, only 38% of patients understand standard drink equivalency. With charts and simple explanations, that jumps to 89%.
That’s why the CDC named alcohol-medication interactions one of five top priorities for medication safety in 2023 - and allocated $15 million to public education campaigns focused on beverage-specific risks.
Bottom Line
It’s not about which drink you choose. It’s about how much alcohol you’re putting in your body - and whether your meds can handle it. Spirits aren’t worse because they’re strong. Beer isn’t safer because it’s weak. Wine isn’t healthier because it’s red.One standard drink of any kind can interfere with your meds. Two can land you in the ER. And if you’re taking a high-risk medication, even one drink is too many.
Ask your pharmacist. Read your label. Use a drink tracker app. And if you’re unsure - don’t drink. Your liver, your brain, and your life are worth more than a glass of wine, a beer, or a shot.
Can I have one glass of wine with my antidepressant?
It depends on the antidepressant. Some, like SSRIs, can cause increased drowsiness or dizziness when mixed with alcohol. Others, like MAOIs, can cause dangerous spikes in blood pressure. Even if your doctor says it’s "okay," start with half a glass and monitor how you feel. Many people find that even small amounts make their meds less effective or worsen side effects like fatigue or brain fog.
Is non-alcoholic beer safe with medications?
Non-alcoholic beer still contains up to 0.5% alcohol. For most people on common meds, that’s not a problem. But if you’re on metronidazole, tinidazole, disulfiram, or certain seizure medications, even that small amount can trigger a reaction. Always check with your pharmacist - especially if you’re on long-term treatment.
Why do some meds say "avoid alcohol" but others don’t?
It depends on how the drug is processed by your body. Medications that are broken down by the liver - like painkillers, sleep aids, and antibiotics - are more likely to interact. Others, like some blood pressure pills, are filtered out by the kidneys and are less affected. But the label might not say everything. Always ask your pharmacist if you’re unsure.
Does it matter if I drink on an empty stomach?
Yes. Drinking on an empty stomach means alcohol hits your bloodstream faster and higher. That increases the chance of dangerous interactions. Food slows absorption, giving your liver more time to process both the alcohol and the medication. Always eat something before drinking - even a snack.
I only drink on weekends. Is that safe?
It depends on the medication. Some drugs build up in your system and stay active for days. If you’re on a long-acting medication like fluoxetine (Prozac) or warfarin, weekend drinking can still interfere with how it works. Even if you don’t drink during the week, the interaction risk remains. Consistency matters more than frequency.
Can alcohol make my medication less effective?
Yes. Alcohol can reduce how well your meds work. For example, it can make antidepressants less effective, reduce the pain relief from NSAIDs, or interfere with antibiotics’ ability to fight infection. It can also make side effects worse - like dizziness or nausea - which might make you stop taking your med altogether.
What should I do if I accidentally mixed alcohol and medication?
If you feel dizzy, nauseous, confused, have trouble breathing, or notice unusual bleeding or bruising, seek medical help immediately. Call your doctor or go to the ER. Don’t wait. Even if you feel fine, it’s worth checking in - some reactions can be delayed. Keep your medication list handy when you go.
Are there any alcohol-free alternatives I can use instead?
Yes. Sparkling water with lime, alcohol-free mocktails, or herbal teas can give you the ritual of a drink without the risk. Many bars now offer quality non-alcoholic options. If you’re drinking for relaxation, try a warm cup of chamomile tea or a walk instead. Your body will thank you.
Next Steps
- Go through your medication list - prescription, over-the-counter, and supplements.
- Ask your pharmacist: "Which of these can’t I mix with alcohol?" Don’t assume they’ll tell you unless you ask.
- Download the GoodRx Alcohol Check app - it’s free and works offline.
- Print a standard drink chart and keep it in your wallet or on your fridge.
- If you’re on a high-risk med, consider switching to alcohol-free weekends - just to be safe.
Alcohol and meds don’t mix - no matter what kind of drink it is. The science is clear. The risks are real. And your health is worth more than a glass of anything.
Joe bailey
November 27, 2025 AT 06:57Man, I never realized one shot could be that dangerous with my sleep meds. I used to think wine was the safe bet. Thanks for laying it out like this - I’m switching to sparkling water after work now. My liver will thank me.
Marissa Coratti
November 28, 2025 AT 09:50It is profoundly concerning that public health messaging around alcohol and pharmaceutical interactions remains so fragmented and anecdotal, despite the overwhelming volume of peer-reviewed clinical data demonstrating dose-independent metabolic competition at the hepatic enzyme level. The normalization of "just one drink" as a benign social ritual obscures the fact that pharmacokinetic interference is not probabilistic - it is mechanistic, inevitable, and often irreversible. We must reframe this not as a matter of personal choice, but as a systemic failure in patient education.
Rachel Whip
November 28, 2025 AT 16:22Just wanted to add - if you're on metronidazole, even a sip of wine or a drop of vanilla extract (which has alcohol) can trigger a reaction. I learned this the hard way after a dentist visit. Always check the fine print on everything, including mouthwash and cough syrup. Your pharmacist is your best friend here.
Amanda Wong
November 29, 2025 AT 23:04Of course the FDA is "catching up" - after thousands of ER visits and preventable deaths. Meanwhile, Big Pharma and Big Alcohol are still cozying up in lobbying offices. This isn’t about safety - it’s about profit margins and keeping people docile with pills and pints.
Stephen Adeyanju
December 1, 2025 AT 10:25So you're telling me my Friday night whiskey with my Xanax is basically playing russian roulette with my brain? Cool cool cool. Guess I'll just stop taking the Xanax then. No big deal. My anxiety will handle it. 🤷♂️
james thomas
December 2, 2025 AT 08:15Bro the whole "standard drink" thing is a scam. Who the hell measures 1.5 oz of whiskey? I pour till it looks right. And beer? I drink 6-pack like it’s water. If your meds can’t handle that, maybe you’re the problem. Also red wine is literally medicine, it’s in the Bible.
Deborah Williams
December 3, 2025 AT 07:35Isn’t it funny how we’ve turned self-medication into a cultural ritual? We drink to unwind, to celebrate, to cope - and then we’re shocked when our bodies rebel. Maybe the real issue isn’t alcohol and pills - it’s a society that outsources emotional regulation to chemistry. Just a thought.
Kaushik Das
December 5, 2025 AT 01:22From India - we don’t have "standard drinks" here. We just drink what’s available. But I’ve seen too many friends with diabetes and high BP get hospitalized after "just one peg." This post is a wake-up call. I’m sharing it with my family tonight. 🙏
Asia Roveda
December 6, 2025 AT 20:34Of course the CDC is spending $15M on this. Meanwhile, our schools can’t afford basic health classes. This is performative activism. Real solutions? Ban alcohol. Ban pills. Ban America. Problem solved.
Micaela Yarman
December 8, 2025 AT 17:38As someone who works in pharmacology, I appreciate the clarity of this post. However, I must emphasize that non-alcoholic beer’s 0.5% ethanol is metabolized differently in individuals with ALDH2 deficiency - common in East Asian populations. Even trace amounts can accumulate. Always disclose your full alcohol history to your provider, no matter how minimal.
mohit passi
December 8, 2025 AT 21:27Alcohol is just another toxin. Your liver doesn't care if it's from a bottle or a bottle of cough syrup. 🍺💊 Just say no to both. Stay clean, stay alive. 🙏
Aaron Whong
December 9, 2025 AT 01:20The ontological framing of alcohol as a singular, homogenous variable is a reductive epistemological fallacy. The phenomenological experience of ethanol ingestion is mediated by polyphenolic matrices, congeners, and beverage-specific pharmacodynamics - which introduces non-linear interaction profiles that cannot be captured by the simplistic 14g standard drink metric. This is pharmacological reductionism masquerading as public health guidance.
Sanjay Menon
December 9, 2025 AT 06:14Wow. This is the most "common sense" thing I’ve read all year. I mean, I’ve been drinking craft IPA with my statins for years. But now that you mention it - maybe I should stop. Or maybe I should just buy a better brand of beer. Quality matters, right?
Joe bailey
December 10, 2025 AT 08:39Replying to @4899 - bro you just used 10 fancy words to say "it’s complicated." I get it. But I just want to know if I can have one beer with my blood pressure med. Can I or not? 🤨