Anaphylaxis from Medication: Emergency Response Steps You Must Know

What Happens During a Medication-Induced Anaphylaxis?
Anaphylaxis from medication is not just a bad reaction-it’s a medical emergency that can kill in minutes. It happens when your immune system overreacts to a drug, triggering a cascade of symptoms that shut down your airway, breathing, and circulation. Common culprits include penicillin, NSAIDs like ibuprofen, chemotherapy drugs, contrast dyes used in scans, and muscle relaxants given during surgery. About 1 in every 10,000 times a medication is given, this reaction occurs. In hospitals, it’s responsible for 20-30% of all anaphylaxis cases.
Here’s the scary part: up to 20% of people having this reaction won’t even get a rash or hives. You might think, ‘No itching, no problem.’ But that’s wrong. The real danger is in what’s happening inside: your throat is swelling, your lungs are tightening, your blood pressure is crashing. Without quick action, you could lose consciousness-or die.
Step 1: Recognize the Signs Before It’s Too Late
You don’t need to see a full-body rash to know something’s wrong. In fact, the most dangerous cases often start quietly. Look for these signs:
- Difficulty breathing or noisy, wheezy breaths (happens in 89% of cases)
- Swelling of the tongue or throat (76% and 82% respectively)
- Hoarse voice or trouble talking (57%)
- Dizziness, fainting, or collapse (49%)
- Pale, clammy skin, especially in children (33%)
If someone just took a new medication-antibiotics, painkillers, or anything else-and suddenly starts having trouble breathing or looks pale and confused, treat it like an emergency. Don’t wait for more symptoms. Don’t ask if they’re sure. Don’t check their phone for allergies. If it looks like anaphylaxis, it is.
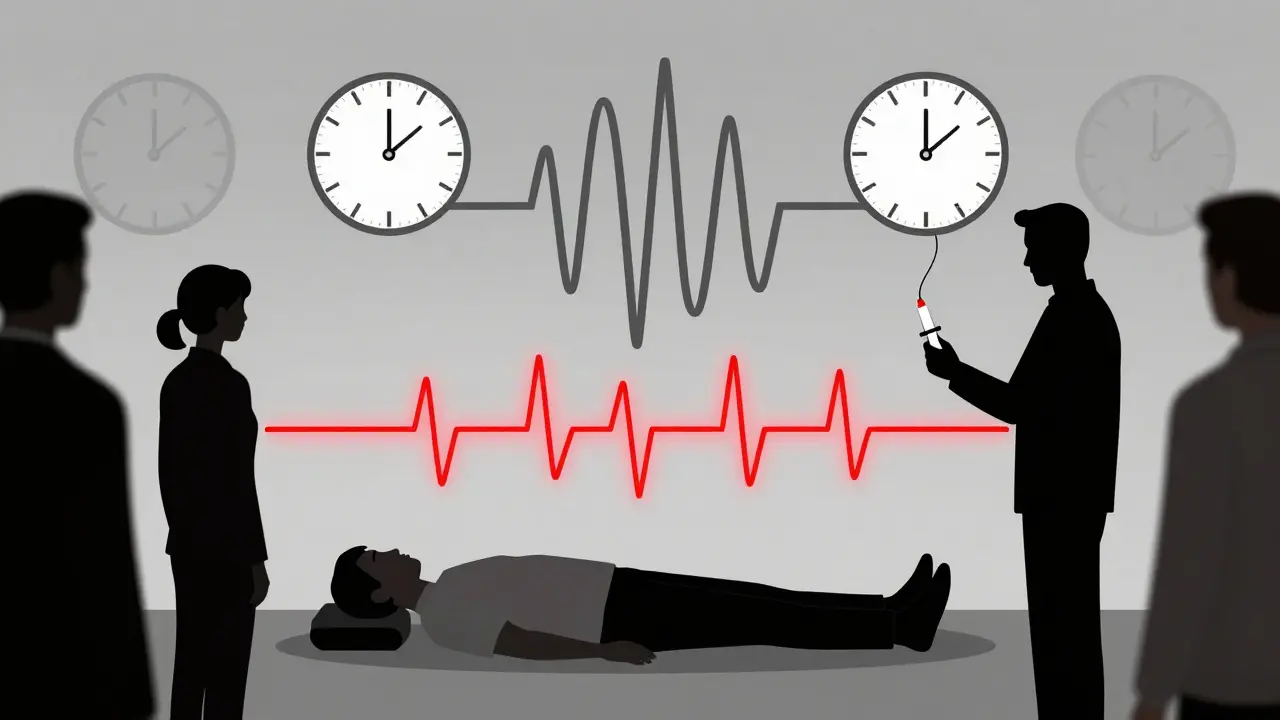
Step 2: Lay Them Flat-No Standing, No Sitting Up
This is one of the most misunderstood steps. If someone is having anaphylaxis, laying them flat is not optional-it’s life-saving. Standing or even sitting upright can cause their blood pressure to drop suddenly, leading to cardiac arrest. Studies show that 15-20% of deaths happen because the person was allowed to stand or walk.
Here’s what to do:
- If they’re conscious and breathing: lay them flat on their back. Elevate their legs slightly if possible.
- If they’re struggling to breathe: let them sit up with legs stretched out. Don’t force them flat if they can’t breathe that way.
- If they’re unconscious: roll them onto their left side (recovery position), especially if they’re pregnant.
- If it’s a child: hold them flat on your lap. Don’t hold them upright.
Every second counts. Don’t waste time trying to make them comfortable. Your job is to keep blood flowing to their brain and heart.
Step 3: Give Epinephrine-Now, Not Later
Epinephrine is the only thing that stops anaphylaxis from killing someone. Antihistamines like Benadryl? They help with itching, but they do nothing for breathing or blood pressure. Steroids? They don’t help in the first hour. Only epinephrine reverses the deadly effects.
Use an auto-injector-EpiPen, Auvi-Q, or Adrenaclick-into the outer thigh. You don’t need to strip clothing. Just jab it through fabric. Hold it in place for 10 seconds. That’s how long it takes to deliver the full dose.
Dosing matters:
- Adults and kids over 30 kg: 0.3 mg
- Children 15-30 kg: 0.15 mg
Don’t wait for symptoms to get worse. Don’t wait for someone else to act. If you’re unsure, give it. Australian data shows that hesitation caused 35% of preventable deaths between 2015 and 2020. The mantra is simple: IF IN DOUBT, GIVE ADRENALINE.

Step 4: Call for Help-Immediately
Epinephrine works fast-but only for 10 to 20 minutes. Symptoms can come roaring back. That’s why you must call emergency services the moment you give the shot. In the UK, dial 999. In the US, dial 911. Don’t wait to see if they improve. Don’t assume they’ll be fine once they’re breathing again.
While you wait for paramedics:
- Keep them lying flat
- Monitor breathing and pulse
- Be ready to give a second dose of epinephrine if symptoms return
Studies show that in hospital settings, it takes an average of 8.2 minutes to give epinephrine after symptoms start. The target? Five minutes. Every minute you delay increases the risk of death.
Step 5: Prepare for a Second Dose-and a Second Wave
One dose isn’t always enough. If symptoms don’t improve-or get worse-after 5 minutes, give a second dose. Some protocols say you can give another every 10 minutes if needed. That’s not reckless. That’s science.
And here’s what most people don’t know: up to 20% of people have a biphasic reaction. That means they seem fine for a few hours, then crash again-sometimes 12, 24, or even 72 hours later. That’s why everyone who has anaphylaxis must be observed in a hospital for at least 4 hours. For medication-induced cases, recent data suggests 6-8 hours may be safer.
Even if they feel fine after the shot, they still need to go to the ER. No exceptions.
Why People Delay-And Why That’s Deadly
Why do so many people wait too long? Fear. Misinformation. Confusion.
Nurses and doctors sometimes hesitate because they’re afraid epinephrine will cause a heart attack. But here’s the truth: out of 35,000 epinephrine doses given for anaphylaxis, only 0.03% caused serious heart problems. Meanwhile, 70% of fatal cases involved no epinephrine at all.
Patients are just as guilty. A 2023 survey found that 68% of people with known allergies carry an auto-injector-but only 41% feel confident using it. Many don’t know how to hold it right. Some inject into fat instead of muscle. Others pull the safety cap off too late. The new Auvi-Q 4.0 has voice guidance to help with this. But you don’t need fancy tech. You just need to know: jab, hold, wait.
Special Cases: What If They’re on Beta-Blockers?
Many adults over 40 take beta-blockers for high blood pressure or heart conditions. These drugs can make epinephrine less effective. In these cases, you may need higher doses-or even multiple doses faster than usual.
There’s no perfect fix. But if someone on beta-blockers has anaphylaxis, don’t hold back. Give the standard dose first. If they don’t improve in 5 minutes, give another. Don’t wait for a doctor. Don’t wait for confirmation. Give it again. Their life depends on it.
What Happens After the Emergency?
After the hospital, the real work begins. You need to find out what caused it. That means allergy testing, usually with a specialist. You’ll likely get a prescription for two epinephrine auto-injectors. Keep one at home. Keep one at work. Keep one in your bag. Never let them expire.
Teach your family, coworkers, even your neighbors how to use them. Write down your triggers and keep a card in your wallet. Make sure your phone’s emergency contacts are set up.
Anaphylaxis from medication doesn’t always happen once. If you’ve had one reaction, your risk of another is higher. But with the right preparation, you can live safely.
Final Rule: Don’t Wait for Perfect Conditions
You won’t always be in a hospital. You might be at home, at school, on a train. There won’t be a doctor nearby. There won’t be a perfect setup. That’s okay. The rules don’t change.
Recognize the signs. Lay them flat. Give epinephrine. Call for help. Be ready to give more. Stay with them until help arrives.
This isn’t about being a hero. It’s about being prepared. Because when seconds matter, you don’t need a medical degree-you just need to act.
Lance Nickie
January 13, 2026 AT 12:27Anny Kaettano
January 13, 2026 AT 23:35I train nurses and med students, and I tell them: if you’re not 100% sure it’s anaphylaxis, you’re still wrong to wait. The symptoms don’t need to be textbook. No rash? Doesn’t matter. Hoarse voice and pale skin? That’s your red flag. Epinephrine isn’t dangerous-it’s the only thing that can flip the switch before the body shuts down. The fear of side effects? Real. But the fear of inaction? Deadlier.
And don’t get me started on beta-blocker patients. I had a 68-year-old man last month who coded because his cardiologist told him to ‘hold off on epinephrine’ until the hospital. He got two doses after 12 minutes. He’s alive now. But he shouldn’t have been in that position at all. If you’re on beta-blockers, your reaction is a ticking clock. Don’t wait for permission. Give it. Give it again. Then give it a third time if needed. Your life isn’t a protocol. It’s yours.
Adam Vella
January 15, 2026 AT 14:57Alan Lin
January 16, 2026 AT 05:34I work in trauma. I’ve held the hand of a 12-year-old who went into cardiac arrest because her mom gave her Benadryl instead of the EpiPen. She didn’t survive. Her mother still calls me every year on the anniversary. Don’t be that person. Don’t be that parent. Don’t be that nurse. If you’re not sure? Give it. If they’re breathing funny? Give it. If they look like they’re about to pass out? Give it. Now. Not in five minutes. Not after you call 911. NOW. Your hesitation isn’t compassion. It’s cowardice dressed up as caution.
Robin Williams
January 18, 2026 AT 00:23Angel Molano
January 18, 2026 AT 23:09mike swinchoski
January 19, 2026 AT 01:24Trevor Whipple
January 20, 2026 AT 22:18Lethabo Phalafala
January 22, 2026 AT 15:28Milla Masliy
January 23, 2026 AT 05:37Damario Brown
January 23, 2026 AT 11:36sam abas
January 24, 2026 AT 20:24Clay .Haeber
January 25, 2026 AT 12:28Priyanka Kumari
January 26, 2026 AT 02:54