CPAP Machines: Types, Mask Fitting, and Adherence Strategies

What CPAP Machines Do and Why They Matter
If you’ve been told you have sleep apnea, you’re not alone. About 22 million Americans have it, and most don’t even know it. CPAP machines are the most effective non-surgical treatment for obstructive sleep apnea - a condition where your airway collapses while you sleep, causing you to stop breathing dozens of times a night. The device delivers steady air pressure through a mask to keep your airway open, stopping those pauses. The result? Fewer awakenings, deeper sleep, and less daytime fatigue. Studies show people who use CPAP consistently cut their risk of heart attack and stroke by 20-30%. But here’s the catch: CPAP machines only work if you use them. And too many people quit within the first few weeks.
The Four Main Types of CPAP Machines
Not all CPAP machines are the same. There are four main types, each designed for different needs and breathing patterns.
- Traditional CPAP delivers one fixed pressure all night. It’s the most basic and cheapest option - usually between $500 and $1,000. Popular models like the ResMed AirSense 10 and Philips DreamStation fall into this category. Good for people with stable breathing patterns and mild to moderate sleep apnea.
- APAP (Auto-Adjusting PAP) changes pressure automatically based on your breathing. If you snore or have an apnea event, it increases pressure. When you’re sleeping peacefully, it drops down. This adaptability makes it more comfortable for many users. Prices range from $1,700 to $3,000. Models like the ResMed AirSense 11 AutoSet are now recommended as first-line therapy by the American Academy of Sleep Medicine, especially if you’re unsure about your ideal pressure or toss and turn a lot.
- BiPAP (Bilevel PAP) gives two different pressures: higher when you inhale, lower when you exhale. This makes breathing feel more natural, especially if you need high pressure (over 15 cm H₂O) or have other lung conditions like COPD. BiPAP machines cost $600-$1,600, but often require a second sleep study to set the right pressures, adding to the cost.
- EPAP (Expiratory Positive Airway Pressure) isn’t a machine - it’s a small, disposable nasal device you insert before bed. It creates resistance when you exhale, helping keep your airway open. It costs $50-$150 per month and works only for mild sleep apnea. Don’t expect it to help if your AHI (apnea events per hour) is over 15.
Market share is dominated by ResMed (45%), Philips Respironics (30%), and Fisher & Paykel (15%). ResMed’s AirSense 11 AutoSet has a 4.7/5 rating from over 1,200 reviews on CPAP.com. Philips DreamStation scores 4.5/5. The difference isn’t just brand loyalty - it’s how well the machine adapts to your night.
Choosing the Right Mask - It’s Not One Size Fits All
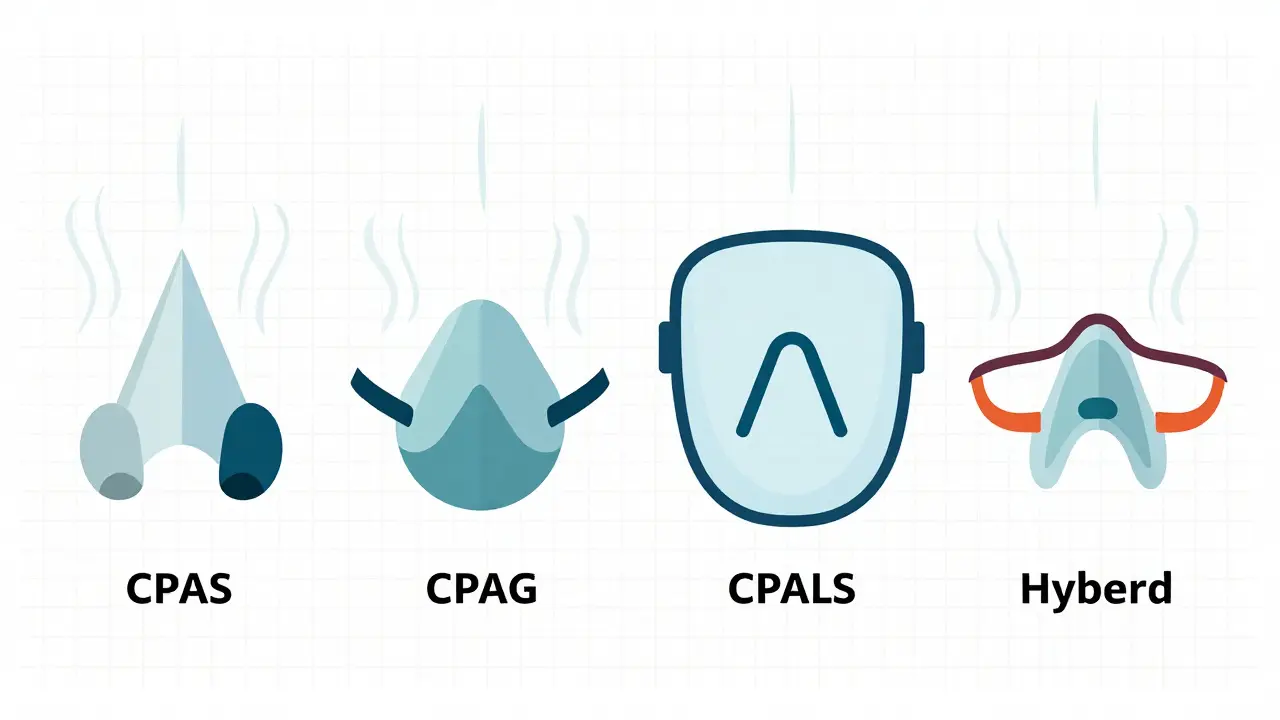
The biggest reason people stop using CPAP? A bad mask fit. According to sleep specialists, 20-30% of users quit because of discomfort, not because the machine doesn’t work. There are four main mask types, and your choice depends on your face shape, sleep position, and breathing habits.
- Nasal pillows sit at the entrance of your nostrils. They’re lightweight, low-profile, and great for side sleepers. Users like u/NasalPillowFan on Reddit say switching from a nasal mask to the AirFit P10 cut their leak rate from 15 to 3 L/min. They’re ideal if you don’t breathe through your mouth.
- Nasal masks cover your nose only. They’re the most popular - used by 45% of CPAP users. Good for people who need higher pressure and breathe through their nose. But they can cause red marks if tightened too much.
- Full-face masks cover both nose and mouth. Essential if you’re a mouth breather or have nasal congestion. But they’re bulkier, harder to seal, and cause more skin irritation. About 35% more users report pressure sores with full-face masks than with nasal pillows.
- Hybrid/oral masks are rare - used by only 5% of users. Designed for people with severe nasal blockages who can’t breathe through their nose at all.
Proper fitting isn’t guesswork. A good sleep clinic will measure your nasal bridge width, cheekbone structure, and facial contours. Even a tiny gap can cause leaks - and leaks mean your pressure drops, and your apnea returns. Acceptable leak rates are under 24 L/min. If your machine shows leaks above that, it’s time to try a different size or style.
Why People Stop Using CPAP - And How to Stay on Track
Despite being 85% effective when used properly, only 46% of users stick with CPAP long-term. Why? The first week is brutal. You feel claustrophobic. Your nose dries out. The machine wakes you up. But most people who quit do it before they give the therapy a real chance.
Here’s what actually works to build adherence:
- Start with daytime practice. Put the mask on while watching TV. Turn on the machine for 5-10 minutes, three times a day. Get used to the feel before you try sleeping.
- Use the ramp feature. This slowly increases pressure over 5-45 minutes so you’re not hit with full force right away. About 75% of users rely on this. Turn it up to 20-30 minutes if you’re struggling to fall asleep.
- Get a heated humidifier. Dry mouth and nose are the #1 complaint. Heated humidification cuts those complaints by 50%. Make sure your machine has one - and set the temperature between 86°F and 95°F.
- Use heated tubing. Cold air in the tube can cause condensation (rainout) and make you wake up. Heated tubing prevents that. Users with it have 78% adherence vs. 52% without.
- Track your data. Modern machines record your usage, AHI, and leak rates. If you see your AHI dropping from 12 to 3 in two weeks, that’s motivation. ResMed’s myAir app gives personalized coaching - users who use it have 27% higher adherence.
Some users swear by CPAP pillows with cutouts for the mask. Others start with just 2 hours a night and slowly add time. The Mayo Clinic says it takes 2-4 weeks to adjust - but 30% of people need three or more mask fittings before they find the right one. Don’t give up after the first bad night.

Travel CPAPs and New Tech on the Horizon
Traveling with a CPAP used to mean lugging a bulky machine. Now, devices like the ResMed AirMini weigh less than a pound and fit in your palm. It’s $650, but it doesn’t have a built-in humidifier - you need to buy the $80 add-on. Noise levels are higher too (52 dBA vs. 30 dBA for standard models). Still, for frequent travelers, it’s a game-changer.
Technology is moving fast. ResMed’s AirSense 11 uses AI to predict apnea events before they happen - reducing AHI by 22% compared to older models. Philips’ DreamStation 3 runs at 25 dBA - quieter than a whisper. Fisher & Paykel’s SleepStyle reduces exhalation pressure by up to 50%, making breathing feel natural. Transcend’s Micro 3 uses transnasal pressure, so you barely feel the mask.
Insurance coverage is changing too. Starting in 2024, Medicare and most private insurers require your machine to track usage. To keep getting coverage, you must use it at least 4 hours a night, 70% of nights. If you fall short, your provider may stop paying. That’s why data tracking isn’t just helpful - it’s necessary.
What to Do If CPAP Isn’t Working
If you’ve tried everything and still can’t stick with it, you’re not failing. CPAP isn’t the only option.
- Try a different mask type. Many people switch from full-face to nasal pillows and suddenly find relief.
- Switch from CPAP to APAP. If your breathing changes at night, auto-adjusting pressure can make a huge difference.
- Consider oral appliances. Custom-fitted devices that move your jaw forward can help mild to moderate cases.
- Explore surgery. Uvulopalatopharyngoplasty (UPPP) or tongue reduction procedures are options for some, but success varies.
- Look into ASV (Adaptive Servo-Ventilation). If you have central sleep apnea - which affects 5-15% of CPAP users - machines like the ResMed AirCurve 10 can help.
Remember: CPAP is the most effective treatment we have. But it’s not magic. It’s a tool. And like any tool, it only works if you use it - and use it right.
Can I buy a CPAP machine without a prescription?
No. In the United States, all CPAP machines require a prescription. This is because they’re classified as Class II medical devices by the FDA. Even if you find one for sale online without a prescription, it’s illegal to sell them that way, and you risk getting the wrong pressure setting - which can be dangerous. Always get a sleep study first.
How long does it take to get used to a CPAP machine?
Most people need 2-4 weeks to adjust. The first few nights are usually the hardest - you might feel claustrophobic, wake up with a dry mouth, or find the noise annoying. But 80% of users who stick with it past the first month report better sleep within 6 weeks. Use ramp mode, heated humidification, and practice with the mask during the day to speed up the process.
Is APAP better than CPAP?
For most people, yes - especially if your breathing changes at night or you’re new to therapy. APAP adjusts pressure automatically, which leads to higher comfort and better adherence. Studies show a 15% higher usage rate compared to fixed-pressure CPAP. But if your sleep apnea is stable and your pressure needs are consistent, a standard CPAP can work just as well - and cost less.
Why does my CPAP mask leak?
Leaks happen when the mask doesn’t seal properly. Common causes: wrong size, wrong type, too tight or too loose, facial hair, or a worn-out cushion. Check your leak rate on your machine’s data screen - anything over 24 L/min means you need to adjust or replace the mask. Try a different style - many users find nasal pillows leak less than full-face masks. Also, make sure you’re cleaning the mask daily; oils from your skin can break down the seal.
Does insurance cover CPAP machines?
Yes - most insurance plans cover 80% of the cost after you meet your deductible. But you’ll need a sleep study diagnosis and a prescription. Many insurers also require proof of use - like 4 hours per night, 70% of nights - to keep covering the machine. Some require prior authorization. Check with your provider before buying.
Can I use a CPAP machine if I have a cold?
You can - but it’s harder. Nasal congestion makes it difficult to breathe through your nose, which is how most masks deliver air. If you’re mouth breathing, you may need a full-face mask. Use saline spray or a decongestant before bed. Keep your humidifier on and clean your mask daily. If you’re too uncomfortable, skip a night or two - but don’t quit. Once you’re better, get back on it.
kenneth pillet
January 18, 2026 AT 15:43Machine doesn't matter if the mask hates you.
Jodi Harding
January 18, 2026 AT 18:10Danny Gray
January 19, 2026 AT 16:56Zoe Brooks
January 20, 2026 AT 20:20Don't give up after the first nightmare night. It gets better. I promise.
Wendy Claughton
January 21, 2026 AT 11:45It’s not about being weak. It’s about finding the right tool. And sometimes, that takes time. And patience. And a lot of trial and error.
Stacey Marsengill
January 22, 2026 AT 10:07Aysha Siera
January 23, 2026 AT 18:48Selina Warren
January 25, 2026 AT 16:54Emma #########
January 26, 2026 AT 17:25It’s not perfect. But it’s worth it.
Andrew McLarren
January 27, 2026 AT 16:48Furthermore, the integration of AI-driven predictive algorithms in newer models represents a significant advancement in therapeutic personalization.
Andrew Short
January 28, 2026 AT 19:08