Dairy Products and Antibiotic Absorption: Timing Matters

When you're sick and prescribed an antibiotic, you're probably focused on getting better. But what you eat with it-especially dairy-can make the difference between healing quickly and fighting the same infection for weeks. It’s not just a myth. Dairy and certain antibiotics don’t mix well, and the science behind it is clear, consistent, and decades old.
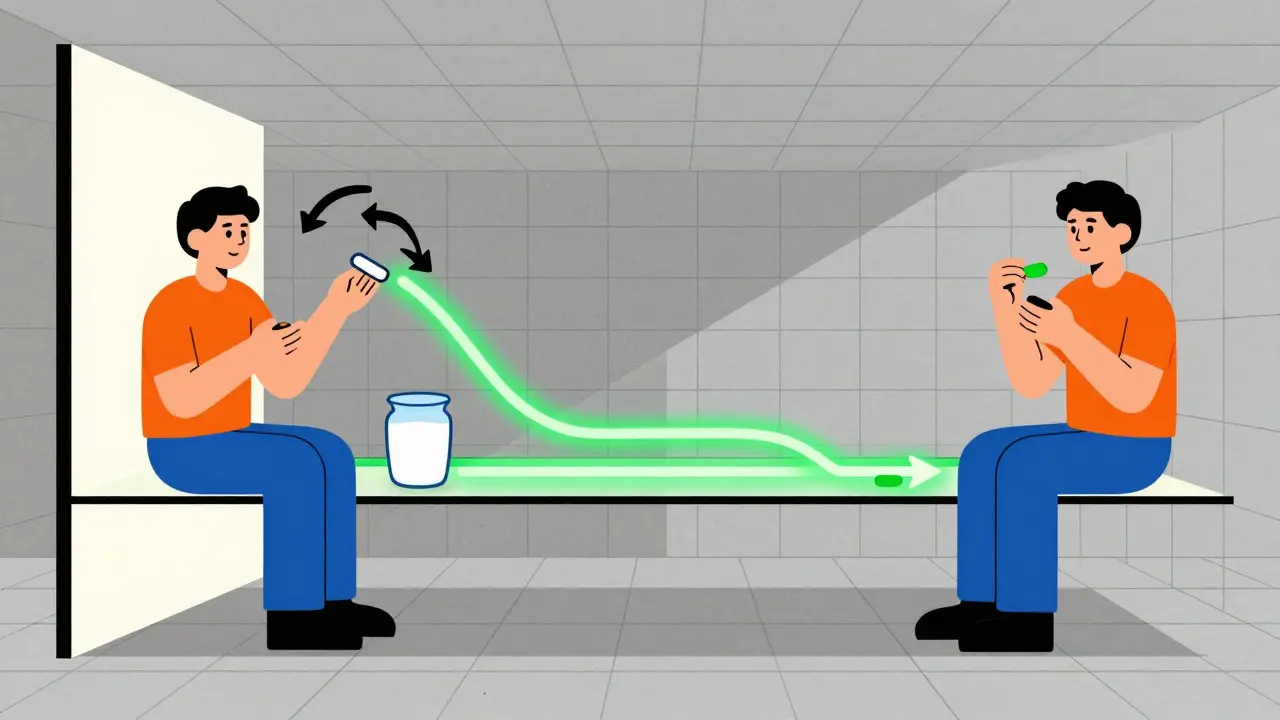
Why Dairy Ruins Some Antibiotics
It all comes down to calcium. Milk, cheese, yogurt, and even calcium-fortified almond or soy milk contain high levels of calcium and other minerals like magnesium and iron. These minerals bind tightly to certain antibiotics in your stomach and intestines, forming what scientists call chelates. These complexes are too big and too stable to be absorbed into your bloodstream. Instead, they pass right through your gut and out of your body-taking the antibiotic with them.
This isn’t a minor issue. Studies show that when you take tetracycline or ciprofloxacin with dairy, your body absorbs anywhere from 20% to 92% less of the drug. That means if you’re supposed to get 500 mg, you might only get 100 mg. That’s not enough to kill the infection. And when antibiotics don’t work as they should, bacteria survive, adapt, and become resistant. This isn’t just about your treatment-it’s part of the bigger crisis of antibiotic resistance.
Which Antibiotics Are Affected?
Not all antibiotics are created equal when it comes to dairy. Two major classes are the most vulnerable:
- Tetracyclines: This group includes tetracycline, doxycycline, and minocycline. Tetracycline is the most sensitive-dairy can cut its absorption by up to 90%. Doxycycline is a bit more forgiving, but still affected. A 2022 study in the Journal of Rawal Academy of Sciences found that even a single glass of milk reduced doxycycline absorption by 40%.
- Fluoroquinolones: This group includes ciprofloxacin (Cipro), levofloxacin (Levaquin), and moxifloxacin (Avelox). These are commonly prescribed for urinary tract infections, sinus infections, and pneumonia. Ciprofloxacin is especially sensitive. Research shows yogurt can slash its absorption by 92%, while milk drops it by 70%.
Other drugs like bisphosphonates (used for osteoporosis) and some antifungals also interact with calcium, but antibiotics are the most common concern because they’re taken for short periods and people often don’t realize the interaction.
Meanwhile, antibiotics like penicillin, amoxicillin, azithromycin, and clindamycin show little to no interaction with dairy. So if you’re on one of those, you’re fine. But if you’re on tetracycline or ciprofloxacin? You need to plan.
How Long Should You Wait?
Timing isn’t just helpful-it’s critical. And the waiting period isn’t the same for every drug.
- Tetracyclines: Take them at least 1 hour before or 2 hours after eating dairy. Some sources recommend up to 3 hours for maximum safety. That means if you take your pill at 8 a.m., don’t have yogurt with breakfast. Wait until after 10 a.m. If you take it at bedtime, avoid cheese or milk at dinner.
- Fluoroquinolones: These need stricter separation. For ciprofloxacin, take it 2 hours before or 4 to 6 hours after dairy. That’s why many people find it easier to take their pill in the morning before eating and then have their milk or yogurt at lunch or dinner.
Why the difference? Tetracyclines bind to calcium quickly but can sometimes be absorbed if separated by just an hour. Fluoroquinolones form even more stable complexes, so you need more time for your stomach to clear out the calcium before the antibiotic arrives.

What Counts as Dairy? (It’s More Than You Think)
Most people think “dairy” means milk, cheese, or yogurt. But calcium is everywhere now.
- Calcium-fortified orange juice
- Plant-based milks (almond, soy, oat, rice) with added calcium
- Calcium-fortified cereals
- Antacids or supplements with calcium carbonate
- Some mineral waters
A 2023 study in the Journal of the American Pharmacists Association found that nearly 30% of patients who thought they were avoiding dairy were still taking their antibiotics with calcium-fortified orange juice or soy milk. And guess what? The interaction was just as bad.
Always check the label. If it says “fortified with calcium,” assume it’s a problem unless your doctor or pharmacist says otherwise.
Real-Life Consequences
This isn’t theoretical. People are getting sick because they didn’t know.
On Reddit, a nurse named NurseAmy87 shared a story about a patient on doxycycline for Lyme disease. She drank milk with every dose. Her symptoms didn’t improve for weeks. Only after her pharmacist asked about her diet did they realize the problem. Once she switched to taking her pill two hours before breakfast, she improved in days.
A Drugs.com user with recurring UTIs had tried three different antibiotics. Nothing worked. Then her pharmacist asked if she ate yogurt after her ciprofloxacin. She did-every night. She stopped. Within a week, her infection cleared.
A 2023 study in the Journal of Patient Experience tracked 200 patients on affected antibiotics. Those who followed the timing rules had a 98% success rate. Those who didn’t? Only 72% got better. And 43% of patients said they were never told about this interaction by their doctor.
What Should You Do?
Here’s your simple, no-fluff action plan:
- Check your prescription. If it’s doxycycline, tetracycline, ciprofloxacin, levofloxacin, or moxifloxacin-stop and read this.
- Ask your pharmacist: “Does this interact with dairy or calcium?” They’re trained for this.
- Plan your meals around your doses. Take the pill on an empty stomach. Wait at least an hour before eating. If it’s a twice-daily dose, take the first dose before breakfast and the second before bed. Avoid dairy at breakfast and dinner.
- Read labels. Calcium-fortified juices, plant milks, and cereals count. So do antacids and supplements.
- If you forget, don’t panic. Skip the dairy that day. Don’t double up on your antibiotic. Just resume the schedule the next day.
The Bigger Picture
This isn’t just about your next cold or UTI. The World Health Organization calls improper antibiotic use one of the top threats to global health. When antibiotics fail because of timing mistakes, bacteria survive. They learn. They mutate. And next time, the drug won’t work-even if you take it perfectly.
The FDA updated labeling rules in January 2023 to make timing instructions clearer on antibiotic bottles. Pharmacies like CVS and Walgreens now include dairy interaction warnings on prescription bags. Digital apps like Medisafe and MyMeds send alerts if you enter ciprofloxacin and then log yogurt.
But the real change has to come from you. You’re the one holding the pill. You’re the one eating the yogurt. And you’re the one who can prevent a failed treatment.
What About New Antibiotics?
Some pharmaceutical companies are trying to fix this. A new version of ciprofloxacin called Cipro XR was designed to be less affected by calcium. But it costs over $200 a prescription-more than 10 times the generic. And even then, it’s not immune.
Researchers are also testing calcium-resistant tetracycline derivatives. One study in the European Journal of Pharmaceutical Sciences (March 2023) showed promising results in lab trials. But they’re still in phase II testing. Don’t expect them before 2026.
For now, the chemistry hasn’t changed. Calcium still binds to these drugs. Your stomach still can’t absorb the chelates. And the only reliable solution? Time. Space. And awareness.
Can I take my antibiotic with a glass of milk if I wait an hour after eating?
No. The problem isn’t just food in your stomach-it’s the calcium still present in your gut. Even if you ate dairy an hour ago, enough calcium remains to bind with tetracyclines and fluoroquinolones. You need to wait at least 2 hours after dairy before taking these antibiotics, and 4-6 hours after for ciprofloxacin. Waiting an hour isn’t enough.
I took my antibiotic with yogurt. Should I take another dose?
No. Don’t double up. Taking extra can cause side effects like nausea, dizziness, or even tendon damage (especially with fluoroquinolones). Instead, skip the next dairy meal and continue the rest of your course as scheduled. Your body will still get enough of the drug over the full course-just don’t repeat the mistake.
Do all dairy products affect antibiotics the same way?
No. Yogurt and hard cheeses have more calcium per serving than milk. In fact, studies show yogurt can reduce ciprofloxacin absorption by 92%, while milk reduces it by 70%. That’s because yogurt is often fortified with extra calcium, and the fermentation process concentrates minerals. Low-fat milk has slightly less calcium than whole milk, but not enough to make a clinical difference.
Can I take calcium supplements with my antibiotic?
Not at the same time. Calcium supplements (like calcium carbonate or citrate) contain the same binding ions as dairy. If you take a calcium pill, wait at least 2 hours before or after your antibiotic. If you’re on a long-term calcium regimen, ask your doctor if you can adjust the timing-like taking the supplement at bedtime and the antibiotic in the morning.
Why don’t doctors always tell patients about this?
Many doctors assume patients know. Others are pressed for time during appointments. A 2022 survey found 43% of patients received no specific warning about dairy interactions. But pharmacists are better trained on this. Always ask your pharmacist when you pick up your prescription. They’re the experts on drug-food interactions.