Diabetes and Thyroid Disease: Overlapping Symptoms and How to Manage Both
When your body’s hormones go out of sync, it doesn’t just cause one problem-it sets off a chain reaction. That’s exactly what happens when diabetes and thyroid disease show up together. These two endocrine disorders don’t just coexist; they talk to each other, often masking each other’s symptoms and making treatment harder. If you have diabetes and suddenly feel more tired than usual, lose weight without trying, or notice your insulin needs have changed for no clear reason, your thyroid might be the hidden culprit.
Why Diabetes and Thyroid Disease Keep Showing Up Together
It’s not coincidence. About 1 in 3 people with diabetes also have a thyroid problem, and nearly 1 in 7 people with thyroid disease have diabetes. The link isn’t random-it’s biological. Both conditions are often driven by the immune system turning against the body. In Type 1 diabetes, the immune system attacks insulin-producing cells in the pancreas. In Hashimoto’s or Graves’ disease, it attacks the thyroid. Because these organs are both part of the endocrine system, the same autoimmune trigger can hit both.
People with Type 1 diabetes are 5 to 10 times more likely to develop thyroid disease than someone without diabetes. Even in Type 2 diabetes, where insulin resistance plays a bigger role, thyroid dysfunction still shows up far more often than it should by chance. Studies show that about 22% of people with thyroid issues also have Type 2 diabetes, compared to just 17% in the general population.
Thyroid hormones directly affect how your body handles sugar. When your thyroid is underactive (hypothyroidism), your body slows down. Glucose metabolism drops by 25-30%, meaning sugar stays in your blood longer. That raises your blood sugar-even if you’re eating the same amount. On the flip side, an overactive thyroid (hyperthyroidism) speeds things up. Your liver releases glucose faster, your muscles use it up quicker, and your body clears insulin more rapidly. That can cause wild swings: high blood sugar one day, low blood sugar the next.
Symptoms That Look Like Diabetes… But Are Thyroid
Many symptoms of thyroid disease look exactly like complications of diabetes. That’s why so many people get misdiagnosed-or worse, undiagnosed.
- Unexplained weight changes: Losing weight without dieting? That’s classic hyperthyroidism. Gaining weight despite eating less? That’s hypothyroidism. But both can be mistaken for poor diabetes control.
- Extreme fatigue: 78% of people with both conditions report constant tiredness. It’s not just from high blood sugar-it’s from low thyroid hormone.
- Hair loss and dry skin: These aren’t just signs of aging or poor diabetes management. Thyroid hormones regulate skin and hair follicle cycles. Low levels = brittle hair, flaky skin.
- Mood swings and depression: Thyroid hormones affect serotonin and other brain chemicals. Depression in diabetics? Check your thyroid.
- Temperature sensitivity: Feeling cold all the time? Hypothyroidism. Sweating through your clothes in a cool room? Hyperthyroidism. Neither should be dismissed as "just diabetes."
Some signs are more unique to thyroid issues: a hoarse voice, muscle cramps, slow reflexes, or trouble remembering things. If you’ve had diabetes for years and suddenly start having memory lapses or your muscles cramp at night, don’t assume it’s nerve damage. Get your thyroid checked.
The Hidden Danger: Hypothyroidism Masking Low Blood Sugar
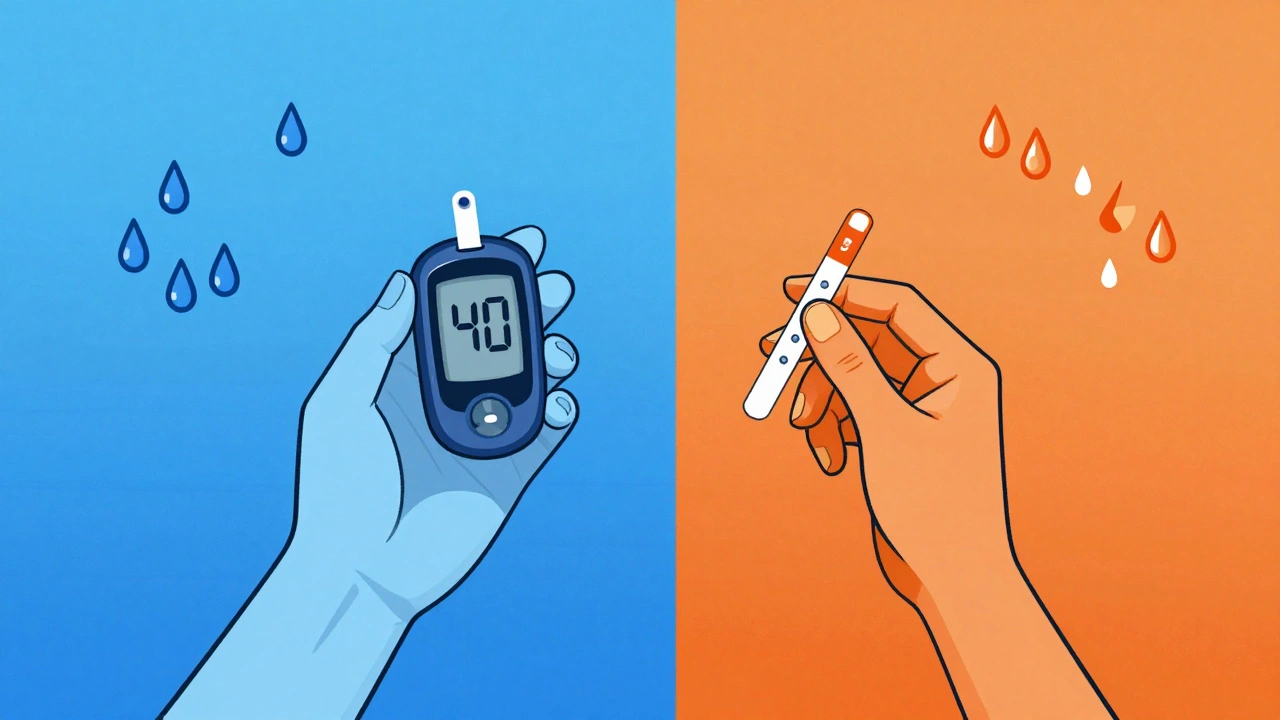
One of the most dangerous overlaps happens when hypothyroidism hides hypoglycemia. Normally, when your blood sugar drops, your body releases adrenaline to warn you-shaking, sweating, racing heart. But hypothyroidism blunts that response. Your body doesn’t send the alarm.
According to clinical data from the Tampa Bay Endocrine Institute, 41% of diabetic patients with untreated hypothyroidism have had at least one episode of severe low blood sugar without warning signs. That’s not just risky-it’s life-threatening. You could pass out before you realize anything’s wrong.
And here’s the twist: when you finally start taking thyroid medication, your body wakes up. Your metabolism speeds up. Your insulin sensitivity improves. Your insulin needs can drop by 20-30% overnight. One patient on DiabetesDaily.com described going from 60 units of insulin a day to 40-within a week of starting levothyroxine-and ending up in the ER with dangerously low blood sugar. That’s why adjusting insulin when thyroid treatment starts isn’t optional-it’s essential.
How Thyroid Problems Make Diabetes Harder to Control
Thyroid dysfunction doesn’t just confuse symptoms-it makes diabetes management more expensive, more dangerous, and more complicated.
People with both conditions have 18.7% higher healthcare costs. Why? Because uncontrolled thyroid disease worsens diabetic complications:
- Retinopathy: T2DM patients with subclinical hypothyroidism have a 37.2% higher risk of developing eye damage.
- Heart disease: Hypothyroidism raises LDL cholesterol by 18-22 mg/dL and triglycerides by 25-30 mg/dL. That’s a double hit-diabetes already raises heart risk. Thyroid makes it worse.
- Nerve damage: Diabetic neuropathy can slow stomach emptying (gastroparesis), which cuts levothyroxine absorption by 15-20%. That means your thyroid meds aren’t working as well, even if you’re taking them correctly.
Hyperthyroidism is no better. It speeds up how fast your body clears insulin. That means you might need 20-30% more insulin just to keep your blood sugar stable. But if your thyroid suddenly becomes normal-say, after treatment-your insulin needs drop fast. Without monitoring, you’re setting yourself up for hypoglycemia.

What You Should Be Doing: A Practical Care Plan
If you have diabetes, you need to be screened for thyroid disease-and vice versa. The American Diabetes Association now recommends that all Type 1 diabetics get a TSH test every year. For Type 2 diabetics with risk factors (family history of thyroid disease, female over 50, or unexplained symptoms), annual testing is also advised.
But annual isn’t enough if you’ve already been diagnosed with thyroid disease. In that case, check your TSH every 3-4 months. Why? Because your insulin needs can shift with your thyroid levels. If your TSH drops from 6.5 to 2.1, your insulin sensitivity is improving. You need to adjust your meds before you crash.
Use a continuous glucose monitor (CGM). A 2022 JAMA study found that diabetics with thyroid disease who used CGMs had 32% fewer low blood sugar events and better time-in-range than those using fingersticks. Why? Because CGMs catch patterns you can’t feel-like overnight dips caused by thyroid changes.
Diet matters too. A Mediterranean diet-rich in olive oil, fish, nuts, vegetables, and whole grains-has been shown in clinical trials to lower HbA1c by 0.8-1.2% and TSH by 0.5-0.7 mIU/L in just six months. That’s two problems, one solution.
Timing your thyroid meds matters. Take levothyroxine on an empty stomach, at least 30-60 minutes before food or coffee. If you have gastroparesis from diabetes, you may need to take it at bedtime instead. Talk to your doctor-this isn’t just a detail, it’s a game-changer.
What Doctors Are Doing Differently Now
Endocrinologists are starting to treat these conditions as one system, not two. The American Association of Clinical Endocrinologists is rolling out new guidelines in late 2024 that include specific algorithms for managing thyroid dysfunction in Type 1, Type 2, and prediabetic patients.
One exciting development: GLP-1 receptor agonists, drugs like semaglutide used for diabetes and weight loss, are showing unexpected benefits for thyroid function. A 2024 pilot study found that 63% of patients with subclinical hypothyroidism saw their TSH levels normalize after 6 months on these drugs-even without thyroid medication.
And research is moving fast. The NIH’s TRIAD study, launched in early 2023, is tracking 5,000 people with autoimmune diabetes to see if early thyroid treatment can prevent or delay diabetes progression. Early signs suggest it might.
Bottom line: if you have diabetes and your symptoms don’t make sense, or your blood sugar keeps acting up for no reason, your thyroid is probably involved. Stop treating them as separate problems. Start treating them as a team.
Can thyroid problems cause high blood sugar even if I’m not eating sugar?
Yes. Hypothyroidism slows down how your body uses glucose, causing sugar to build up in your blood-even if you’re eating a low-carb diet. Your liver may also release more glucose than usual. This isn’t about diet-it’s about hormone imbalance.
Should I get tested for thyroid antibodies if I have Type 2 diabetes?
Yes, especially if you have unexplained fatigue, weight gain, or a family history of autoimmune disease. While Type 1 diabetes is strongly linked to autoimmune thyroid disease, about 1 in 5 Type 2 patients also have thyroid antibodies, which means they’re at higher risk for developing full-blown thyroid disease later.
Why does my insulin dose keep changing without any lifestyle changes?
Your thyroid may be the reason. Hyperthyroidism increases insulin clearance, so you need more. Hypothyroidism improves insulin sensitivity, so you need less. If your insulin needs shift suddenly and you haven’t changed your diet, activity, or weight, check your TSH and thyroid antibodies.
Can treating my thyroid help my diabetes get better?
Absolutely. Correcting thyroid dysfunction often leads to better blood sugar control, lower insulin needs, fewer hypoglycemic episodes, and slower progression of complications like nerve and eye damage. Treating your thyroid isn’t just about energy or weight-it’s about protecting your whole metabolic health.
What’s the best way to monitor both conditions at home?
Use a continuous glucose monitor (CGM) to track blood sugar patterns and a home TSH test kit (available through many labs) to check thyroid levels every 3-4 months if you’re on treatment. Keep a journal of symptoms-fatigue, mood, weight, temperature sensitivity-and share it with your doctor. Patterns matter more than single numbers.
Sean McCarthy
December 1, 2025 AT 23:17Diabetes and thyroid issues are a nightmare combo. I had both and didn't know it for years. My sugar kept spiking even when I ate nothing. Turned out my TSH was 8.5. Once I started levothyroxine, my insulin needs dropped 30%. No joke.
Jaswinder Singh
December 3, 2025 AT 19:47You people act like this is some big secret. My aunt had this and the doctors kept blaming her diet. She lost 20 pounds in 3 months and they said she was just "not trying." Then her TSH came back and they were silent. This is medical negligence.
Courtney Co
December 5, 2025 AT 15:56I feel you so hard. I cried in my car after my endo told me my fatigue wasn't "real" because my HbA1c was "fine." Then I got my TSH results and realized I'd been walking around with a dead battery for two years. My skin was flaking, my hair was falling out, I couldn't wake up. And they called it "diabetic burnout."
Now I'm on meds and I feel human again. But why did it take 18 months? Why is this not standard screening? Why are we still treating these like separate problems?
I just want someone to listen. Not fix. Not diagnose. Just hear me.
James Steele
December 7, 2025 AT 02:18The pathophysiological interplay between the hypothalamic-pituitary-thyroid axis and pancreatic beta-cell function is profoundly underappreciated in clinical endocrinology. The bidirectional modulation of insulin sensitivity via T3-mediated upregulation of GLUT4 translocation and hepatic gluconeogenesis suppression is not merely coincidental-it's a systemic regulatory cascade.
Moreover, the subclinical hypothyroidism-induced dyslipidemia exacerbates the atherogenic profile inherent in metabolic syndrome, thereby amplifying cardiovascular risk stratification beyond conventional Framingham metrics.
It's not just about TSH-it's about FT3, FT4, reverse T3, and thyroid peroxidase antibodies. Yet most primary care providers still treat TSH as a binary on-off switch. This is 2024, not 1999.
Louise Girvan
December 7, 2025 AT 02:21They don't want you to know this. Big Pharma doesn't profit from fixing the root cause. They profit from insulin, from metformin, from thyroid meds, from CGMs, from lab tests. They want you dependent. This article? It's a trap. It's designed to make you think you're getting help while they keep selling you pills.
Have you tried fasting? Have you tried cold exposure? Have you tried removing gluten? No? Then you're still part of the system.
soorya Raju
December 8, 2025 AT 04:27lol u think its the thyroid? i bet its the 5g towers or the fluoridated water. my cousin in delhi got diabetes after his phone exploded. now he cant even walk. thyroid? nah. its the chemtrails man. they put it in the air to make us weak. then they sell us insulin to fix it. genius right?
also i typed this on my phone so srry for typos. my hands are cold from the conspiracy.
Dennis Jesuyon Balogun
December 9, 2025 AT 03:57This is the truth many of us live with but never speak. In Nigeria, we don't have access to TSH tests regularly. We feel tired, we lose weight, we gain weight, our sugar goes wild-and we blame ourselves. We think we're failing. We're not. Our systems are failing us.
If you're reading this and you're a doctor, please screen your patients. If you're a patient, demand the test. Don't wait for permission. Your body is not broken. It's screaming.
We are not alone. We are not weak. We are survivors.
Grant Hurley
December 9, 2025 AT 04:12Been there. My doc said "just give it time" when I said my insulin kept changing. I ignored it for 6 months. Then I started using a CGM and saw my sugar dropping at 3am every night. Turns out my TSH was 7.9. Started meds, adjusted insulin, and now I'm sleeping through the night for the first time in years.
Don't wait. Get tested. Even if you think you're fine.
Nnaemeka Kingsley
December 10, 2025 AT 21:49bro this is real. my uncle had diabetes for 10 years. then he started getting cold all the time and his hair fell out. doc said it was aging. i made him get tested. TSH was 12. he started meds and now he's walking again. he says he feels like his old self.
if you have diabetes and something feels off? trust your gut. get your thyroid checked. it's simple. it's cheap. it could save your life.
Kshitij Shah
December 10, 2025 AT 21:53So let me get this straight. You're telling me that after decades of being told to count carbs and take insulin, the real issue was my thyroid the whole time? Wow. I guess I could've just skipped the whole diabetes thing and started taking levothyroxine in 2015. Saved a lot of money. And a lot of shame.
Bee Floyd
December 11, 2025 AT 05:12My endo finally said it: "Your insulin needs are shifting because your thyroid is waking up." I didn't even know my thyroid was asleep. Now I track my TSH every 90 days and adjust my basal rates accordingly. It's not magic. It's medicine. And it's working.
Thank you for writing this. I needed to see it in writing.
Jeremy Butler
December 12, 2025 AT 21:47It is axiomatic that the endocrine system functions as a unified regulatory apparatus, wherein perturbations in one component necessarily engender compensatory or dysregulatory responses in adjacent systems. The concomitant manifestation of autoimmune thyroid disease and type 1 diabetes mellitus represents not a coincidence, but a manifestation of polyglandular autoimmune syndrome type 2, a well-documented entity in the literature since the 1950s.
Yet, the persistence of fragmented, organ-specific paradigms in clinical practice remains a profound failure of medical integration. The time for siloed endocrinology has expired.
Shashank Vira
December 12, 2025 AT 21:52Let me be the first to say it: this article is a masterpiece of medical storytelling. The way it weaves molecular biology with lived experience-T3’s effect on GLUT4 translocation, the silent erosion of hypoglycemic awareness, the quiet tragedy of hair falling out in the shower-it reads like poetry written by a scientist who has wept in the clinic. This isn’t just information. This is a lifeline.
And the GLP-1 agonist findings? That’s the future. Not just treatment. Transformation.