Difference Between Medication Side Effects and Allergic Drug Reactions
It’s easy to think that if a drug makes you feel sick, you’re allergic to it. But that’s not always true. In fact, most people who say they’re allergic to a medication aren’t. They’re just experiencing a side effect - something completely different from a real drug allergy. This mix-up isn’t just confusing; it can be dangerous. It can lead to worse treatments, higher costs, and even life-threatening infections. So what’s the real difference? And why does it matter so much?
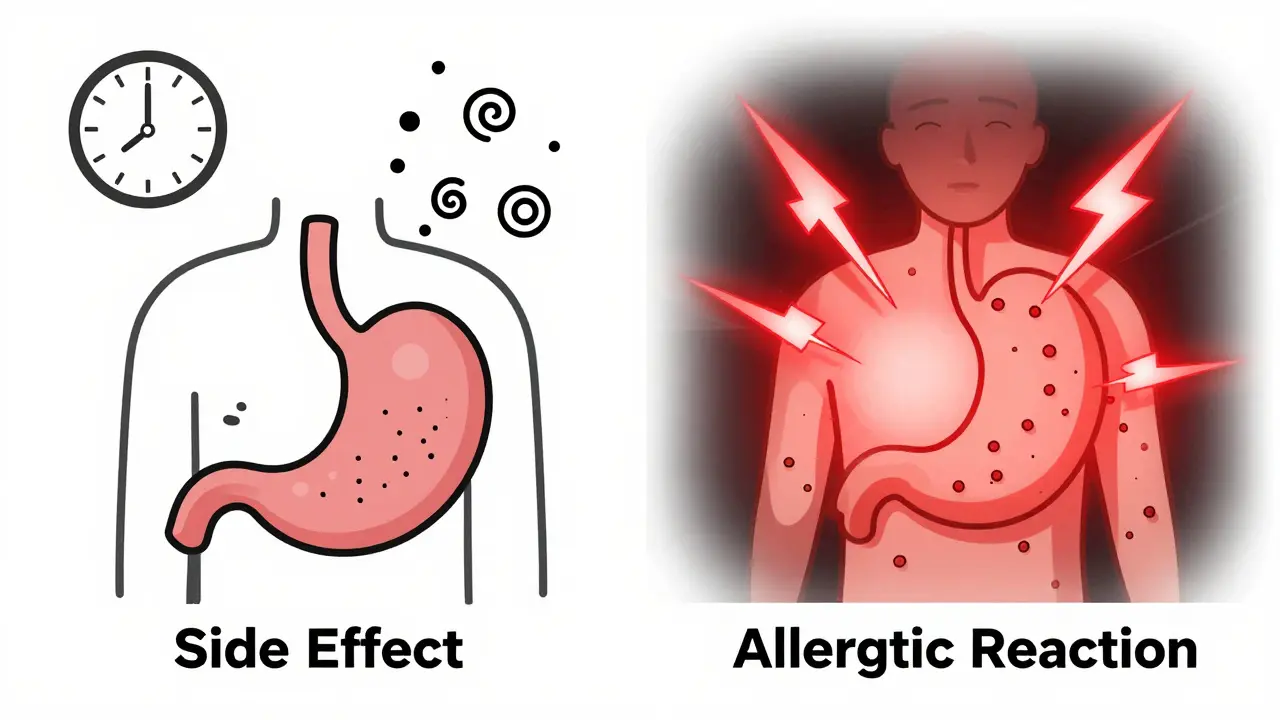
What Are Medication Side Effects?
Side effects are predictable, known reactions to how a drug works in your body. They’re not caused by your immune system. They’re caused by the drug’s chemistry doing things it wasn’t meant to do - like irritating your stomach, drying out your mouth, or messing with your muscle function. These reactions are listed in the drug’s official paperwork, often with percentages. For example, statins cause muscle aches in about 5-10% of users. Metformin, a common diabetes drug, gives 20-30% of people stomach upset.These reactions usually show up within hours or days of starting the drug. But here’s the good part: they often get better over time. Your body adjusts. About 70-80% of common side effects fade within two to four weeks. That’s why doctors sometimes tell you to keep taking the medicine even if you feel a little off at first. Taking metformin with food cuts GI side effects in 60% of people. A cough from lisinopril? Switching to another blood pressure pill usually fixes it.
Side effects can be managed. You can lower the dose. You can take it with food. You can add another drug to counter it. They’re inconvenient, sometimes annoying, but rarely dangerous - unless you ignore them and push through severe symptoms like chest pain or extreme dizziness.
What Is a True Allergic Drug Reaction?
An allergic reaction is your immune system going haywire. It sees the drug as an invader - like a virus or pollen - and attacks it. This isn’t about how the drug works. It’s about your body’s overreaction. These reactions are rare. Only about 5-10% of all bad drug reactions are true allergies, according to the American Academy of Allergy, Asthma & Immunology.There are two main types. Immediate reactions happen fast - within minutes to two hours. These are IgE-mediated. Symptoms include hives, swelling of the lips or throat, trouble breathing, or anaphylaxis. Anaphylaxis is life-threatening. It affects 0.05-0.5% of drug exposures, and even with treatment, 0.3-1% of cases are fatal. Delayed reactions take longer. They show up one to two weeks later, often as a rash. Maculopapular rashes (flat red spots with bumps) are the most common, appearing in 90% of these cases.
Penicillin is the big one. About 80% of severe drug allergies are to penicillin or related antibiotics. But here’s the twist: 80-90% of people who say they’re allergic to penicillin aren’t. They had a stomachache or a rash years ago and assumed the worst. When tested properly - with skin tests or blood tests - most turn out to be fine. That’s why mislabeling is such a problem.
Key Differences at a Glance
| Feature | Side Effect | Allergic Reaction |
|---|---|---|
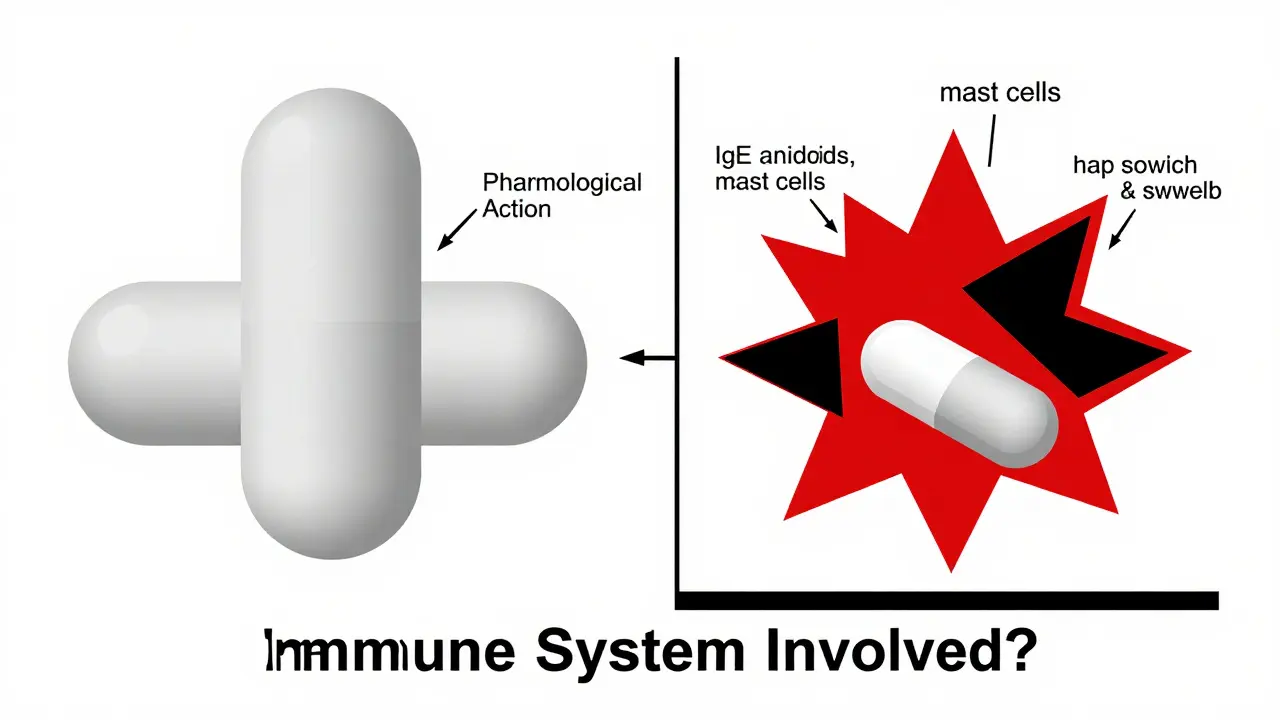
| Caused by | Drug’s pharmacological action | Immune system response |
| Immune system involved? | No | Yes |
| Timing | Hours to days; often improves over time | Immediate (minutes) or delayed (days to weeks) |
| Dose-dependent? | Usually yes - higher dose, worse effect | No - happens at normal doses |
| Common symptoms | Nausea, dizziness, headache, dry mouth, muscle aches | Hives, swelling, wheezing, anaphylaxis, rash |
| Can it be managed? | Yes - dose change, timing, other meds | No - must avoid completely |
| Testable? | No | Yes - skin tests, blood tests (IgE, BAT) |
Why Mislabeling Is a Big Deal
If you’re told you’re allergic to penicillin and you’re not, you’ll likely get a different antibiotic - one that’s broader, stronger, and more expensive. These drugs kill more good bacteria, increase the risk of C. diff infections, and contribute to antibiotic resistance. A 2021 JAMA Internal Medicine study found that patients wrongly labeled as penicillin-allergic have a 69% higher risk of getting a dangerous MRSA infection.The cost? About $4,000 more per patient per year. In the U.S. alone, mislabeled drug allergies cost the system $1.1 billion annually. Hospitals see longer stays - 0.5 to 1.5 extra days per admission. And it’s not just penicillin. People avoid statins because they think a headache is an allergy. They skip NSAIDs because of a stomach ache. They refuse antibiotics for ear infections because they once got a rash after a different drug.
Doctors have to use second-line drugs, which are less effective, more toxic, and harder to prescribe. That’s not just expensive - it’s risky. And it’s all based on a misunderstanding.
How to Tell the Difference - What to Look For
Not all reactions are clear-cut. But here’s how to start sorting them out:- Timing matters. Did symptoms start within 1-2 hours? That’s a red flag for allergy. Did they start after a week? Could be a delayed reaction - still likely allergic. If it took 3 days and it’s just nausea? Probably a side effect.
- Symptoms matter. Hives? Swelling? Trouble breathing? That’s an allergy. Nausea? Diarrhea? Dizziness? That’s a side effect.
- History matters. Did you have the same reaction every time you took the drug? Or was it just once? Did you take it again later and it was fine? If it was a one-time thing and you’ve taken it since without issue, it’s likely not an allergy.
- Family history doesn’t matter. Just because your mom is allergic to penicillin doesn’t mean you are. Allergies aren’t inherited like eye color.
And here’s the thing: if you’ve been told you’re allergic to a drug but never got tested, you might be wrong. The CDC recommends a three-step process for penicillin: 1) Review your history, 2) Skin test (97% accurate at ruling out allergy), 3) Oral challenge (if safe). Only 0.2% of low-risk patients react during the challenge.

What You Can Do - Real Steps for Patients
You don’t need to be a doctor to make a difference. Here’s what you can do:- Don’t assume. If you think you’re allergic to a drug, write down exactly what happened - when, what symptoms, how long it lasted.
- Ask for a referral. If you’ve been labeled allergic to penicillin, ask your doctor about allergy testing. Most primary care providers can refer you to an allergist.
- Update your records. If you’ve been tested and cleared, make sure your doctor and pharmacy know. Ask for your medical record to be updated.
- Carry a card. If you have a confirmed allergy, carry a medical alert card or bracelet. But if you’re not sure - don’t assume.
One patient in Bristol told me she avoided all antibiotics for 15 years because she thought she was allergic to penicillin after a rash as a child. At 42, she got tested - negative. She took amoxicillin for a sinus infection last year. No issues. Her doctor called it the best $200 she ever spent.
What Doctors Are Doing About It
Hospitals are waking up. In 2018, only 15% of U.S. hospitals had programs to clear up false drug allergy labels. By 2023, that jumped to 65%. Academic hospitals are leading the way - 85% have formal programs. Community hospitals? Only 45%.Electronic health records now have alerts that pop up when a patient has a penicillin allergy listed. They ask: “Has this been confirmed?” If not, they suggest testing. A 2023 study showed that using these alerts improved documentation accuracy by 40-60%.
There’s also new tech. The basophil activation test (BAT), approved by the FDA in 2023, is more accurate than skin tests alone. And for some drugs, like abacavir (used for HIV), genetic testing for HLA-B*57:01 is now standard. It cuts allergic reactions from 8% to 0.4%.
But there’s still a gap. Only 10% of U.S. allergists can handle the volume of drug allergy evaluations needed. That’s why training primary care doctors is key. Programs that teach them how to spot false allergies have boosted correct documentation by 55%.
What’s Next
The goal? Reduce mislabeled allergies by 50% by 2027. That’s the American College of Allergy, Asthma & Immunology’s target. And it’s doable. Every time someone gets tested and cleared, they get better treatment. Hospitals save money. Antibiotics stay effective. Lives get saved.Understanding the difference between side effects and allergies isn’t just medical knowledge. It’s personal safety. If you’ve ever been told you’re allergic to a drug - and you’ve never been tested - you owe it to yourself to find out. You might be carrying a label that’s holding you back. And you might not even know it.
Can you outgrow a drug allergy?
Yes, especially with penicillin. About 80% of people who had a true penicillin allergy in childhood lose it over 10 years. That’s why testing later in life is so important. Just because you reacted once doesn’t mean you always will.
Is a rash always a sign of allergy?
No. Many rashes from drugs are side effects, not allergies. Viral infections, heat, or even the drug itself can cause a rash without immune involvement. If the rash appears after a week and you feel fine otherwise, it’s more likely a side effect. But if it’s itchy, spreading, or comes with swelling or breathing trouble - get help right away.
Can you have a reaction the first time you take a drug?
Yes. Unlike pollen allergies, drug allergies don’t need prior exposure. Your immune system can mistake the drug for a threat the very first time you take it. That’s why some people have anaphylaxis on their first dose of penicillin - even if they’ve never taken it before.
What if I’m allergic to one antibiotic, am I allergic to all?
Not necessarily. Penicillin allergies don’t mean you’re allergic to all antibiotics. Only certain classes are cross-reactive. For example, if you’re allergic to amoxicillin (a penicillin), you might react to ampicillin, but not to azithromycin or doxycycline. Always get tested before assuming.
Are there tests to confirm a drug allergy?
Yes. For penicillin, skin testing is the gold standard - 97% accurate at ruling out allergy. Blood tests like the basophil activation test (BAT) are newer and also reliable. For delayed rashes, patch testing may be used. But there’s no universal test for all drugs. Diagnosis often combines history, testing, and sometimes a controlled challenge under medical supervision.
Can side effects turn into allergies?
No. Side effects and allergies are different biological processes. A stomach ache from metformin won’t become an allergic reaction. But you can develop a true allergy to a drug you’ve taken before - even if you never had a problem. That’s why it’s important to report any new reaction, even if you’ve used the drug safely in the past.
Ansley Mayson
February 1, 2026 AT 14:35Bob Hynes
February 2, 2026 AT 10:34