Hypothyroidism vs. Hyperthyroidism: Key Differences and Treatments
When your thyroid acts up, it doesn’t just make you tired or anxious-it can throw your whole body off balance. Two common but opposite conditions, hypothyroidism and hyperthyroidism, affect millions of people, especially women, and often go undiagnosed for years. One slows you down. The other speeds you up. And yet, their symptoms can look so similar that even doctors miss them at first.
What’s Really Going On With Your Thyroid?
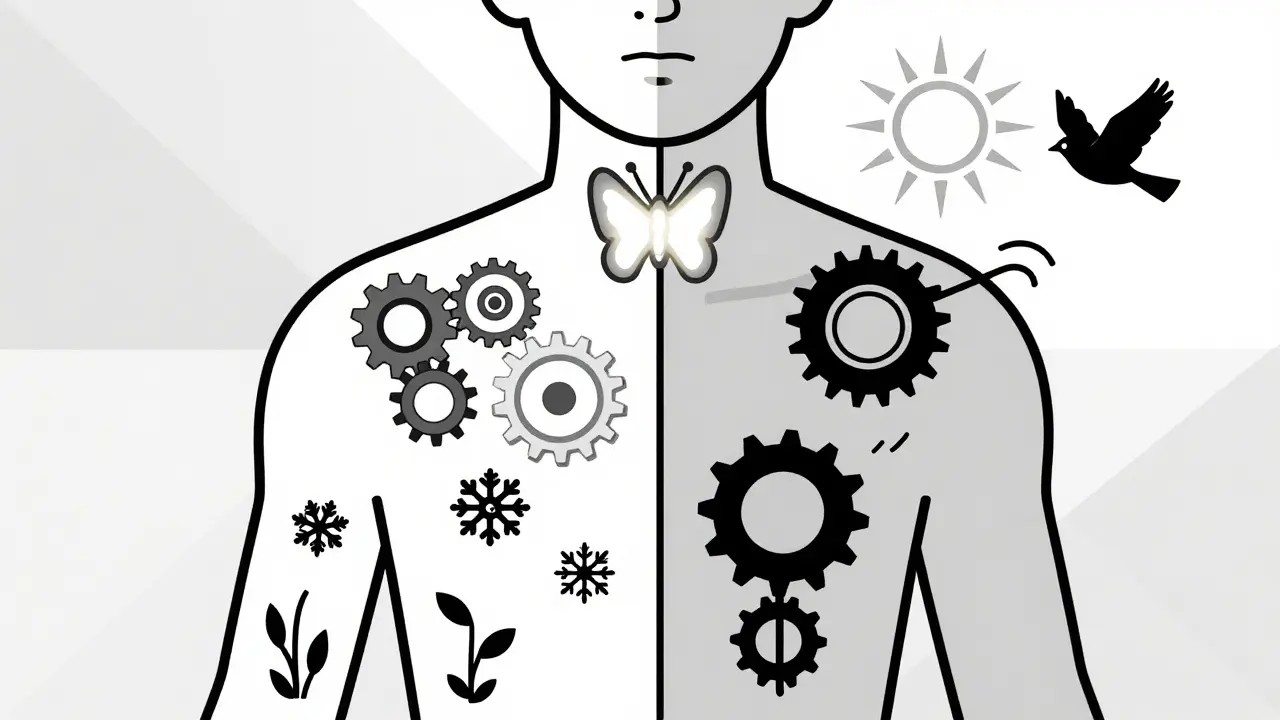
Your thyroid is a small butterfly-shaped gland at the base of your neck. It makes two hormones-T4 and T3-that control how fast your cells use energy. Think of it like a thermostat for your metabolism. If it’s underactive, everything runs slow. If it’s overactive, everything runs hot. Hypothyroidism means your thyroid isn’t making enough hormones. About 4.6% of U.S. adults have it, and most cases come from Hashimoto’s thyroiditis-an autoimmune disease where your immune system attacks your own thyroid. Hyperthyroidism, on the other hand, means your thyroid is making too much. Around 1.2% of Americans have this, and most of those cases are caused by Graves’ disease, another autoimmune condition where your body accidentally tells your thyroid to overproduce. Both are more common in women-up to 8 times more likely than in men. And while symptoms can show up at any age, hypothyroidism becomes much more common after 50, especially in women. Hyperthyroidism tends to hit earlier, between 20 and 40, but it also shows up in older adults, often in sneaky ways.How Do You Know If You’re Slowing Down or Speeding Up?
The symptoms of these two conditions are like night and day-but they’re easy to confuse because fatigue, weight changes, and mood swings happen in both. With hypothyroidism, your body feels like it’s running on low battery:- You gain 10 to 30 pounds even if you eat the same as before
- You’re always cold-even in summer
- Your skin gets dry, your hair falls out, and your nails become brittle
- You feel sluggish, depressed, or foggy-brained
- You’re constipated more often
- Your periods become heavier and more frequent
- Your heart rate drops below 60 beats per minute
- You lose weight even if you’re eating more
- You’re always hot, sweating even in cool rooms
- Your heart races-even when you’re sitting still
- You feel nervous, anxious, or like you’re on edge
- Your hands shake
- You have frequent bowel movements or diarrhea
- Your periods become lighter or stop altogether
- Your heart rate climbs above 100 beats per minute
How Doctors Diagnose It
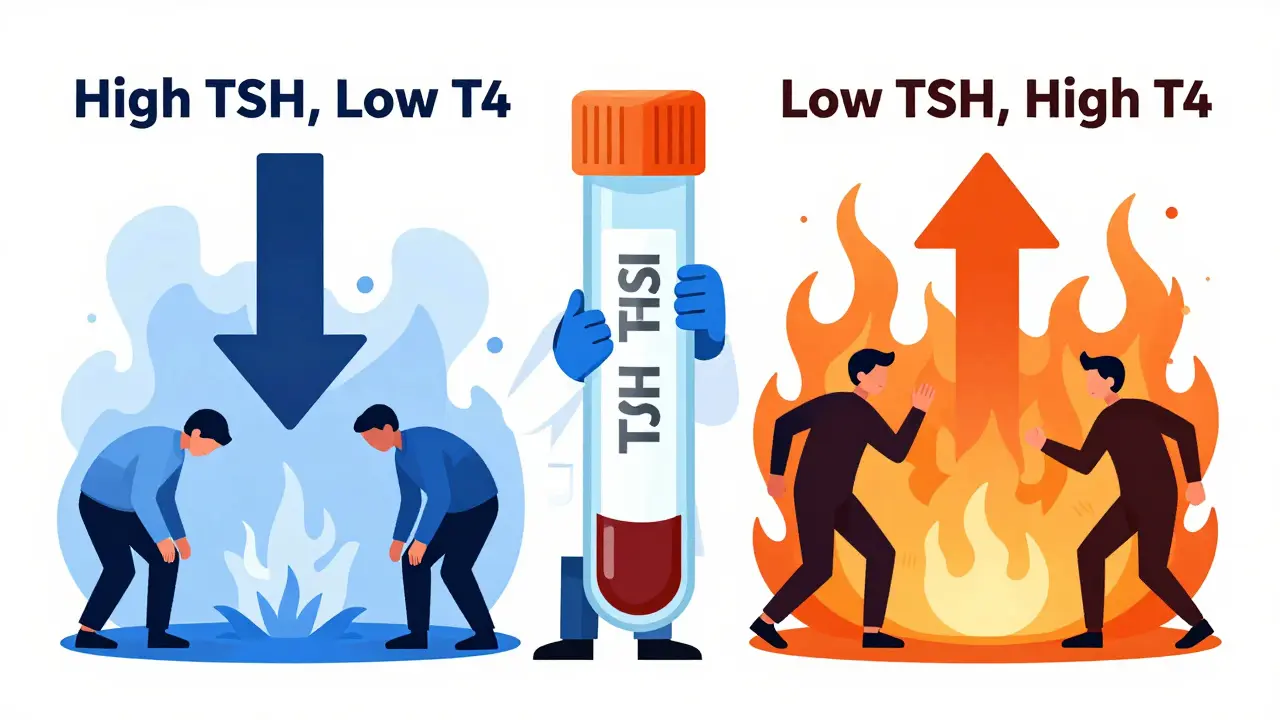
You can’t diagnose this by symptoms alone. Too many other things-stress, sleep issues, depression, menopause-can mimic thyroid problems. That’s why blood tests are non-negotiable. The first test is always TSH-thyroid-stimulating hormone. It’s made by your pituitary gland and tells your thyroid when to work harder or slow down.- In hypothyroidism, TSH is high (usually above 4.5 mIU/L) because your brain is screaming at your thyroid to make more hormones. Free T4 is low.
- In hyperthyroidism, TSH is low (usually below 0.4 mIU/L) because your brain sees too much thyroid hormone and shuts off the signal. Free T4 and T3 are high.
Treatment: One Is Simple. The Other Is Complicated.
If you have hypothyroidism, treatment is straightforward: daily levothyroxine, a synthetic version of T4. The standard dose is about 1.6 mcg per kilogram of body weight. For a 70kg person, that’s around 112 mcg per day. It takes 6 to 8 weeks for the full effect. You’ll get your TSH rechecked every 6 to 8 weeks until it’s stable. Once it is, you’ll usually just need a check-up once a year. But here’s the catch: 15% of people don’t absorb it well-especially those with celiac disease, or who take it with coffee, calcium, or iron. It must be taken on an empty stomach, at least 30 to 60 minutes before breakfast. And 45% of patients admit they skip doses because of lifestyle conflicts. About 15% of hypothyroid patients have genetic differences that make it hard to convert T4 into active T3. For them, adding T3 (like Cytomel) sometimes helps-but it’s not standard, and most doctors won’t prescribe it unless symptoms persist despite normal labs. Now, hyperthyroidism is trickier. You can’t just add more hormone. You have to slow down or shut off the overproduction. Three main options:- Antithyroid drugs: Methimazole (5-60 mg/day) or propylthiouracil (PTU). These block hormone production. Methimazole is first-line because it’s safer and taken once daily. But it carries a small risk of liver damage (1 in 2,000) and a rare but serious drop in white blood cells (1 in 500). Blood tests every month are required.
- Radioactive iodine (RAI): You swallow a capsule. The radiation destroys part of your thyroid. It’s effective, simple, and permanent. But 80% of people end up with hypothyroidism within a year and need lifelong levothyroxine. It’s not used in pregnant women or young children.
- Thyroid surgery: Removing part or all of the thyroid. Usually reserved for very large goiters, cancer suspicion, or if drugs and RAI don’t work. Recovery takes weeks, and you’ll need thyroid hormone replacement afterward.
What Happens If You Don’t Treat It?
Untreated hypothyroidism can lead to high cholesterol, heart disease, infertility, and in extreme cases, myxedema coma-a life-threatening drop in body temperature, heart rate, and breathing. It’s rare, but fatal if not treated immediately. Untreated hyperthyroidism can cause atrial fibrillation (a dangerous heart rhythm), bone loss, and thyroid storm-a medical emergency where your heart races over 140 bpm, you have high fever, vomiting, and confusion. Mortality is 10-20% without ICU care. Both conditions can wreck your quality of life. A 2022 study in the Journal of Occupational and Environmental Medicine found untreated hypothyroidism costs $1,200-$2,500 per year in lost productivity. Hyperthyroidism? Even more-$3,500 to $6,000 annually due to testing, meds, and procedures.
jesse chen
December 28, 2025 AT 07:17I’ve been on levothyroxine for 7 years, and honestly? The biggest issue isn’t the meds-it’s the coffee. I used to take it with my morning brew, and I felt like a zombie. Once I switched to taking it with water, 30 minutes before breakfast? Life changed. I’m not saying this is magic, but… it’s something. Also, don’t skip the annual TSH check. Even if you feel fine. I learned that the hard way.
Alex Ragen
December 29, 2025 AT 23:56One must ask: is the thyroid truly the thermostat-or merely a proxy for the deeper, existential dissonance between our metabolic desires and the cold machinery of biological determinism? We are told to ‘fix’ the gland, yet we ignore the ontological weight of fatigue-how it is not merely a symptom, but a metaphysical echo of a civilization that demands perpetual motion. Levothyroxine? A bandage on the wound of modern alienation.
Lori Anne Franklin
December 31, 2025 AT 20:18OMG I’m so glad someone wrote this!! I had my thyroid checked after 3 years of feeling like I was underwater all the time. My doctor said ‘it’s just stress’… until I begged for TSH. Turns out my TSH was 18. I cried in the parking lot. Now I take my pill like a sacred ritual-no coffee, no calcium, no excuses. You’re not lazy. You’re not broken. You’re just hypothyroid. And it’s fixable.
Zina Constantin
January 2, 2026 AT 18:41As someone who traveled to 12 countries in two years while managing Graves’ disease, I can tell you this: hyperthyroidism doesn’t care about your itinerary. I was diagnosed after collapsing in a Tokyo subway. My heart rate was 148. No fever. No chest pain. Just pure, unrelenting panic. RAI saved my life-but I had to learn to live with hypothyroidism after. It’s not the end. It’s a new chapter. And yes, you still get to travel. You just need to pack extra pills.
Sarah Holmes
January 4, 2026 AT 17:22How is it possible that in 2025, we still treat thyroid disorders like a second-tier medical concern? The fact that doctors routinely dismiss fatigue as ‘stress’ or ‘menopause’ is not negligence-it’s systemic misogyny. Women’s pain is pathologized, ignored, or labeled ‘psychosomatic.’ I’ve seen four doctors before one finally ordered a TSH. My TSH was 27. I was 31. This is not ‘common.’ This is criminal.
Jay Ara
January 6, 2026 AT 02:50bro i had hyperthyroidism in 2020… lost 20 lbs in 3 months, couldnt sleep, hands shaking like i was in a quake… doc said its anxiety. i went to another doc after 6 months… tsh was 0.02. rai worked but now i take pill daily. its fine. just get tested. dont wait.
Michael Bond
January 7, 2026 AT 20:46Levothyroxine works. But only if you take it right.
Kuldipsinh Rathod
January 8, 2026 AT 00:50my aunt had graves disease and she said the bulging eyes were the worst part… not the heart racing or weight loss… just looking in the mirror and not recognizing yourself. it’s like your body betrays you in ways you can’t hide.
SHAKTI BHARDWAJ
January 9, 2026 AT 00:15you people are so naive. thyroid is just a distraction. the real problem is that modern life is poison. glyphosate, plastics, fluoride, gluten. your thyroid is just screaming for help. no pill will fix that. you need to go raw, live in a cabin, drink rainwater, and meditate in silence. or you’re just part of the problem.
Matthew Ingersoll
January 10, 2026 AT 13:35Resmetirom’s early data is promising, but we need long-term studies. The thyroid is a complex endocrine organ-not a broken faucet. Treating it like one risks oversimplifying the entire hormonal axis. We’re still learning how T3 conversion, gut health, and cortisol interact. Until then, caution over enthusiasm.