Linezolid & Tyramine: Managing Hypertension Risk and Diet
Tyramine Intake Calculator for Linezolid Patients
Calculate Your Daily Tyramine Intake
Your Current Intake
Key Takeaways
- Linezolid blocks monoamine oxidase (MAO) enough to make tyramine‑rich foods dangerous.
- Consuming >100 mg of tyramine while on linezolid can trigger a hypertensive crisis.
- Restrictions start 24 h before treatment, continue through therapy, and last about 2 weeks after stopping.
- Typical culprit foods: aged cheeses, tap beer, red wine, fermented soy, air‑dried meats.
- Provide patients with a visual food list, blood‑pressure checks, and clear written guidance.
What is Linezolid?
Linezolid is an oxazolidinone‑class antibiotic approved by the FDA in 2000 for serious Gram‑positive infections such as MRSA and VRE. It works by preventing bacterial ribosomes from starting protein synthesis, a mechanism that makes it highly effective against multidrug‑resistant pathogens.
Beyond its antibacterial action, linezolid also has a side‑effect profile that matters to anyone prescribing or taking the drug. At therapeutic doses (600 mg twice daily) it inhibits both MAO‑A and MAO‑B by roughly 40‑50 %, acting as a weak, reversible MAO inhibitor.
How Linezolid Inhibits Monoamine Oxidase
Monoamine oxidase (MAO) is the enzyme that breaks down dietary amines like tyramine. By dampening MAO activity, linezolid lets tyramine linger in the bloodstream, where it can cause a sudden surge in norepinephrine and blood pressure.
Clinical studies from the University of Toronto showed a 1.8‑fold increase in tyramine‑induced pressor response compared with placebo-about 85 % of the effect seen with moclobemide, a dedicated MAO‑A inhibitor. The inhibition is reversible; MAO activity usually returns to baseline within 24-48 hours after stopping the drug.
Tyramine - The Food Culprit
Tyramine is a naturally occurring monoamine found in aged, fermented, or improperly stored foods. It competes with norepinephrine for the same transporters, and when MAO is blocked, tyramine can cause a rapid rise in vascular tone.
Typical tyramine content (mg per 100 g): aged cheddar ≈ 150, blue cheese ≈ 900‑1500, tap beer ≈ 120, red wine ≈ 50, fermented soy (e.g., miso) ≈ 80. The FDA and IDSA guidelines advise staying below 100 mg per day while on linezolid.
Why Hypertensive Reactions Occur
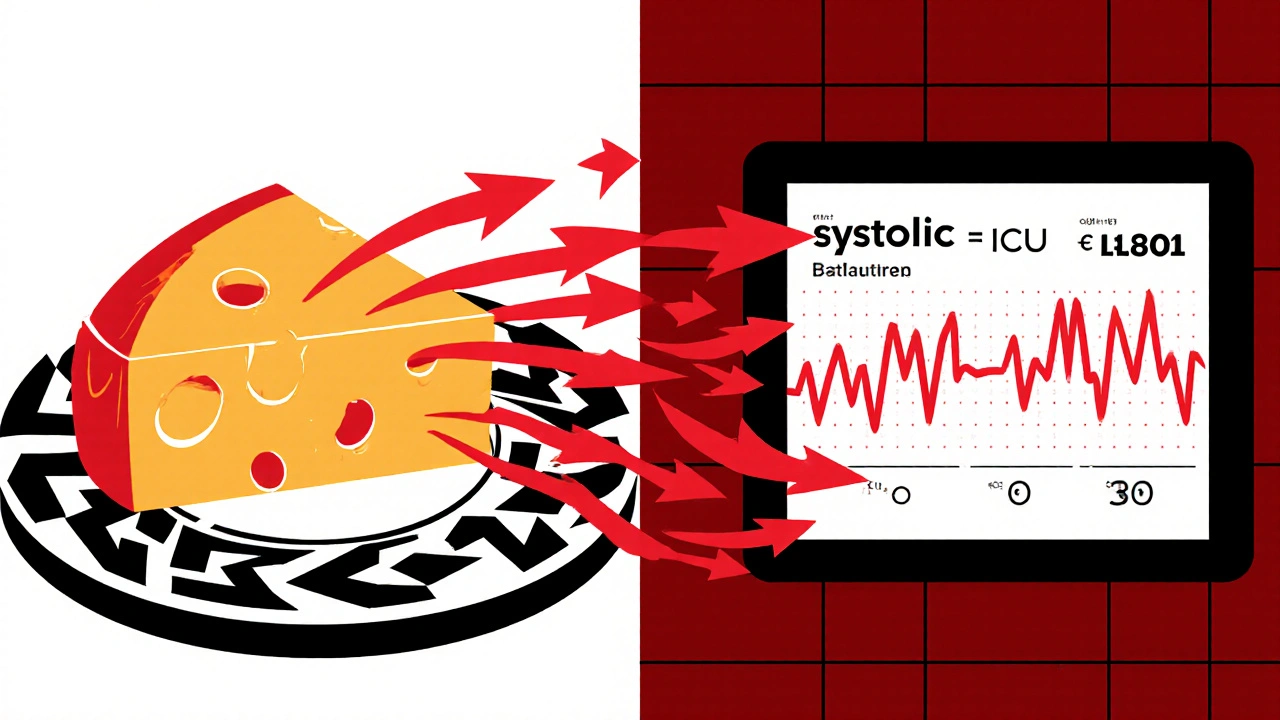
When a patient eats a high‑tyramine meal, the excess tyramine isn’t broken down quickly because MAO is partially inhibited. The result is a spike in circulating norepinephrine, which contracts blood vessels and pushes systolic pressure well above 180 mmHg. Documented cases show pressures ranging from 185‑248 mmHg, often requiring ICU care and rapid‑acting antihypertensives.
Risk factors that amplify the reaction include pre‑existing hypertension, obesity (higher BMI was linked to greater tyramine sensitivity in the Toronto study), and concurrent serotonergic medications that can add to the catecholamine surge.
Clinical Evidence of Linezolid‑Tyramine Hypertension
Between 2018‑2023 the FDA’s adverse‑event database captured 1,247 linezolid‑related hypertension reports (≈ 4.3 % of all linezolid events). A 2021 Journal of Antimicrobial Chemotherapy review identified 17 severe hypertensive crises over five years, with 65 % needing ICU admission.
Case reports highlight the timeline: a patient on linezolid developed a hypertensive emergency after eating aged cheddar; blood pressure only dropped after linezolid discontinuation, normalizing 26 days later. The reversible nature of MAO inhibition means the risk fades after the drug clears, but clinicians must continue restrictions for roughly two weeks post‑therapy.
Managing the Diet: Practical Steps
- Start early: educate the patient 24 hours before the first dose.
- Provide a visual guide: a one‑page chart listing foods and their approximate tyramine content (e.g., "1 oz aged cheddar ≈ 150 mg").
- Set a clear threshold: advise “no foods that exceed 100 mg of tyramine per day.”
- Monitor blood pressure: baseline measurement, then twice‑daily checks for patients with known hypertension.
- Extend the restriction: keep the diet for 14 days after the last linezolid dose.
Electronic health record alerts can remind prescribers and pharmacists to hand out the diet sheet. Involving a dietitian improves adherence, especially for long‑course therapy (>2 weeks).

Medication Interactions to Watch
Because linezolid blocks MAO, other agents that increase catecholamines or serotonin can cause dangerous synergy. Common culprits include:
- Serotonergic antidepressants (SSRIs, SNRIs) - risk of serotonin syndrome.
- Sympathomimetics such as pseudoephedrine or phenylephrine - additive pressor effect.
- Dopaminergic drugs (e.g., levodopa) - unpredictable blood‑pressure swings.
When possible, switch to alternatives or pause the interacting medication for the duration of linezolid therapy.
Future Outlook: New Antibiotics Without MAO Inhibition
Researchers are developing oxazolidinones that retain antibacterial potency but lack MAO activity. Contezolid (MRX‑I) is in Phase III trials and shows promise as a linezolid‑free option for resistant Gram‑positive infections.
Even as newer agents arrive, linezolid remains a cornerstone for MRSA and VRE. Keeping the dietary protocol sharp is essential, especially as outpatient use grows and patients self‑manage their meds at home.
Quick Checklist for Clinicians
- Screen for hypertension before starting linezolid.
- Give written tyramine‑restriction guide at prescription.
- Set up blood‑pressure monitoring schedule.
- Review all current serotonergic or sympathomimetic drugs.
- Re‑educate patient 48 h after discharge (if inpatient).
Frequently Asked Questions
Can I eat any cheese while on linezolid?
No. Most aged cheeses contain more than 100 mg of tyramine per serving. Stick to fresh, non‑fermented cheeses like mozzarella or cottage cheese.
How long after stopping linezolid do I need to avoid tyramine?
The safe window is about 14 days after the last dose, reflecting the time needed for MAO activity to recover.
What blood‑pressure level is considered a hypertensive crisis?
A reading of ≥180 mmHg systolic or ≥120 mmHg diastolic, especially if symptoms like headache, chest pain, or vision changes appear.
Do over‑the‑counter cold medicines interact with linezolid?
Many contain pseudoephedrine, a sympathomimetic that can raise blood pressure. Choose a decongestant without pseudoephedrine or hold it until linezolid finishes.
Is the risk the same for all patients?
Risk is higher in people with existing hypertension, high BMI, or those taking serotonergic drugs. Younger, normotensive patients generally tolerate modest tyramine intake better, but the precaution still applies.
linezolid tyramine interaction is a real safety concern, but with clear patient education, a simple dietary chart, and routine blood‑pressure checks you can prevent life‑threatening spikes while still delivering the antibiotic’s life‑saving benefits.
Pamela Clark
October 25, 2025 AT 18:33Oh, because we all love a good list of forbidden cheeses while battling superbugs, right?
Greg Galivan
October 25, 2025 AT 19:56Listen, the data is crystal clear – you cant just hand out a flyer and hope patients read it. The risk is real and you need stricter monitoring.
Anurag Ranjan
October 25, 2025 AT 21:20Start the diet education 24 h before linezolid. Give patients a simple chart with foods under 100 mg tyramine. Check BP twice daily if they have hypertension.
James Doyle
October 26, 2025 AT 18:33From a pharmacodynamic perspective, linezolid’s partial inhibition of monoamine oxidase A and B introduces a quantifiable risk vector that necessitates a systems‑level mitigation strategy. The clinical literature consistently demonstrates a 1.8‑fold augmentation of tyramine‑elicited pressor responses relative to placebo, situating the drug within the same safety envelope as reversible MAO‑A inhibitors. Consequently, the practice of providing patients with a granular tyramine‑content matrix is not merely a pedagogical nicety but a requisite component of risk management. Moreover, the temporal dynamics of MAO reconstitution post‑therapy-approximately 24‑48 hours for enzymatic activity normalization-imply that the restriction window must be extended to account for lingering pharmacologic effects. Empirical evidence from adverse‑event reporting systems indicates that over 4 % of linezolid recipients experience hypertensive sequelae, with a non‑trivial proportion progressing to ICU admission. This epidemiologic signal underscores the imperative for proactive blood pressure surveillance, especially in cohorts with baseline hypertension or elevated body mass index. The integration of electronic health record alerts can operationalize this surveillance, prompting clinicians to dispense printed dietary guides at the point of prescription. In parallel, interdisciplinary collaboration with dietitians facilitates adherence by contextualizing the tyramine threshold within culturally appropriate food patterns. Finally, awareness of synergistic interactions with serotonergic and sympathomimetic agents-such as SSRIs and pseudoephedrine-must be woven into the therapeutic decision‑making algorithm to preempt additive pressor effects. In sum, a multifaceted approach encompassing patient education, pharmacovigilance, and interprofessional coordination is essential to mitigate linezolid‑induced hypertensive crises.
Edward Brown
October 26, 2025 AT 19:56Sure, but have you considered that the pharma giants deliberately downplay these risks to keep profits high? They push linezolid as a miracle drug while quietly lobbying against stricter labeling. It's all part of a larger agenda to control the narrative on antibiotic safety. Think about it.
ALBERT HENDERSHOT JR.
October 26, 2025 AT 22:43Great points everyone. 📈 I’d add that a collaborative care plan, involving pharmacists, nurses, and dietitians, can streamline the education process and ensure consistent follow‑up. Using a standardized checklist helps keep nothing out of sight, and patients appreciate the clarity. Let’s keep sharing best practices! :)
Suzanne Carawan
October 27, 2025 AT 00:06Oh absolutely, because a checklist will magically stop anyone from eating aged cheddar on a Saturday night. 🙄
Kala Rani
October 27, 2025 AT 01:30i dont think this is even a big deal
Donal Hinely
October 27, 2025 AT 02:53Whoa, calm down! You’re basically saying we should just ignore a known life‑threatening interaction. That’s reckless, not chill.