Psychiatric Medication Combinations: Generic Alternatives and Real-World Risks
When one psychiatric medication isn’t enough, doctors often add another. This isn’t experimental-it’s standard practice. About 30-40% of people with major depression don’t respond to the first drug they’re given, according to the landmark STAR*D trial. So clinicians turn to combinations: an SSRI with an atypical antipsychotic, an SNRI with buspirone, or bupropion paired with an SSRI to fix sexual side effects. These combinations can boost remission rates by up to 20%. But here’s the catch: switching from brand-name drugs to generics in these mixtures can break the balance-and sometimes, it breaks the patient.
Why Combination Therapy Works (and When It’s Necessary)
Combining medications isn’t about over-treating. It’s about precision. For someone with treatment-resistant depression, adding a low dose of aripiprazole (Abilify) to escitalopram (Lexapro) can be the difference between staying stuck and finally feeling better. The FDA approved this combo in 2014 after trials showed 24.3% remission with the combination versus just 11.2% with placebo plus antidepressant.
Another proven pairing is Symbyax-olanzapine and fluoxetine in one pill. It was designed specifically for people who haven’t responded to antidepressants alone. For anxiety, adding buspirone to sertraline helps with lingering worry without the risk of dependence that comes with benzodiazepines. And for those suffering from SSRI-induced sexual dysfunction, swapping in bupropion can restore intimacy without losing antidepressant benefits-60-70% of patients see improvement, per a 2001 study in the Journal of Clinical Psychiatry.
These aren’t random guesses. They’re based on how the drugs interact with brain chemistry. But each combination is like a finely tuned engine. Change one part, even slightly, and the whole system can sputter.
The Generic Switch: A Hidden Risk
The FDA says generics are just as good as brand names. They must contain the same active ingredient and fall within an 80-125% bioequivalence range. Sounds fair, right? Except when you’re talking about psychiatric meds.
In 2019, a study of nearly 28,500 patients found those switched from brand-name SSRIs to generics had a 22.3% higher rate of treatment failure. Why? Because bioequivalence isn’t bio-identical. A 45% difference in absorption can mean the difference between a stable mood and a relapse.
Take lithium. It’s used for bipolar disorder and has a razor-thin therapeutic window: 0.6-1.2 mmol/L in the blood. Too low, and mania returns. Too high, and you get tremors, confusion, even kidney damage. A 2018 case series from the University of British Columbia documented three patients who went from stable to manic within two weeks of switching from Eskalith to a generic lithium. Their blood levels dropped from 0.85 to 0.55 mmol/L-even though the dose didn’t change.
And it’s not just lithium. Generic bupropion XL (Wellbutrin XL) has been flagged by the FDA since 2012. Over 137 adverse event reports linked the generic versions to breakthrough anxiety, panic attacks, and depression. Why? Because the extended-release beads don’t release the drug the same way. One manufacturer’s beads dissolve too fast. Another’s too slow. The result? Unpredictable blood levels.
Venlafaxine ER: A Hidden Trap in Combination Therapy
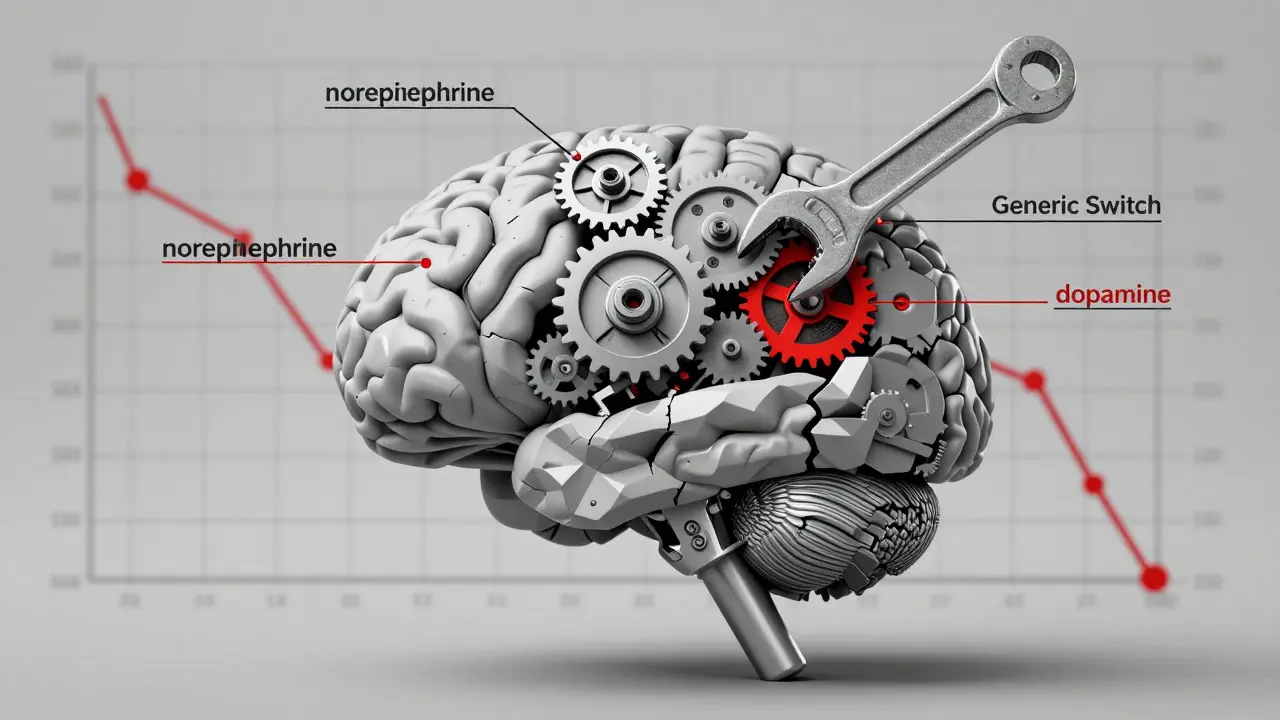
Venlafaxine ER (Effexor XR) works by balancing serotonin and norepinephrine in a precise 2:1 ratio. That ratio matters. Change it, and you lose efficacy-or get worse side effects.
Generic versions use different bead technologies. Some use osmotic systems. Others use multiparticulate beads. These differences alter how the drug is released over time. In combination therapy-say, venlafaxine plus aripiprazole-this small shift can destabilize the whole treatment. Patients report sudden anxiety, insomnia, or emotional numbness after switching to a generic they didn’t even know was different.
One RN on GoodRx described a patient who developed severe akathisia-restlessness so intense it felt like being inside a vibrating cage-just 10 days after switching from brand Effexor XR to a generic fluoxetine. The patient ended up hospitalized. The connection? A subtle change in how the drugs were absorbed together.
What Patients Are Saying Online
Real stories don’t show up in clinical trials. They show up on Reddit, PatientsLikeMe, and Drugs.com.
On r/depression, a May 2023 thread titled “Generic switch ruined my carefully balanced med cocktail” got over 1,200 upvotes. Comments like “Switched from Lamictal to Apotex generic and my Zoloft stopped working” and “After generic Abilify, my obsessive thoughts came back full force” are common.
On PatientsLikeMe, 38.7% of patients on combination therapy reported worsened symptoms after a generic switch. That’s nearly 4 in 10. Compare that to just 12.3% of people on single medications.
And the worst offender? Generic bupropion XL. On WebMD, 68% of negative reviews mention “inconsistent effects,” “mood swings,” or “sudden crashes.” Meanwhile, some patients report no issues-but those stories are drowned out by the ones where things went wrong.
How Doctors Are Trying to Protect Patients
Some clinics have started fighting back. The Massachusetts General Hospital Psychopharmacology Program recommends three steps before switching:
- Measure baseline symptoms using tools like the MADRS scale.
- Only switch when the patient is stable-not during a crisis.
- Follow up within 7-10 days to catch early warning signs.
The University of Toronto built a risk tool that gives points for things like narrow therapeutic index (3 points), multiple drug interactions (2 points), and past bad reactions to generics (4 points). If the score hits 6 or higher, the system flags it for the doctor’s review.
Documentation matters too. A 2021 case report showed that identifying the exact generic manufacturer-Aurobindo vs. Mylan-solved unexplained toxicity in a patient on lithium and carbamazepine. That’s how precise this gets.
And yes, it takes time. A 2022 survey of 327 psychiatrists found managing a generic switch in combination therapy takes 45-60 minutes across multiple visits. Monotherapy? Just 15-20 minutes.
Who’s Pushing for Change-and Who’s Pushing Back
On one side: insurers and pharmacy benefit managers. Generics make up 89% of psychiatric prescriptions by volume. They’re cheaper. In 2022, the generic psychotropic market hit $18.7 billion.
On the other side: psychiatrists, pharmacists, and patients. In 2023, the FDA proposed tighter bioequivalence standards-90-111% instead of 80-125%-for extended-release psychotropics used in combinations. That’s a direct response to over 120 citizen petitions from psychiatric groups.
Some states are acting. California’s AB 1477, effective January 2023, requires pharmacists to notify prescribers when substituting generics in patients on multiple psychiatric drugs. Michigan saw a 22% drop in ER visits after passing a similar law.
The Department of Veterans Affairs now mandates that veterans stabilized on combination therapy must stay on the same generic manufacturer for at least 12 months. Preliminary data shows an 18.7% drop in psychiatric hospitalizations.
And now, authorized generics-brand-name drugs sold without the brand name-are becoming more common. Symbyax’s authorized generic launched in 2022. It’s the same pill, just cheaper. For patients on complex combinations, this might be the safest middle ground.
What You Should Do If You’re on Combination Therapy
If you’re taking two or more psychiatric medications:
- Ask your doctor: Is this combination approved for my condition?
- Ask your pharmacist: Which manufacturer made this generic? Is it the same as last time?
- Never let a pharmacy switch your meds without telling you. Ask for a copy of the prescription label.
- Track your symptoms. Use a mood journal or app. Note changes in sleep, energy, anxiety, or thoughts.
- If you feel worse after a switch-call your doctor immediately. Don’t wait. Don’t assume it’s “just adjustment.”
- Request therapeutic drug monitoring if you’re on lithium, valproate, or carbamazepine. Blood tests are non-negotiable.
And if your doctor says, “It’s just a generic-it’s the same thing”-ask them this: Would you switch your own medication without telling you? If they hesitate, that’s your answer.
The Future: Personalized Medicine and Better Standards
The FDA plans to release product-specific bioequivalence guidelines for 27 high-risk psychiatric combinations by 2025. That’s a big step. So is the rise of pharmacogenetic testing-checking your genes to predict how you’ll metabolize a drug. One expert predicts this will cut adverse outcomes by 60% within five years.
But until then, the system is still broken. Cost-cutting shouldn’t come at the cost of mental stability. A $5 savings on a pill isn’t worth a hospital stay, a lost job, or a suicide attempt.
The truth? Not all generics are created equal. And when you’re on combination therapy, the differences matter more than ever.
Hilary Miller
January 21, 2026 AT 23:16Margaret Khaemba
January 23, 2026 AT 07:48Malik Ronquillo
January 23, 2026 AT 23:19Brenda King
January 24, 2026 AT 07:38Daphne Mallari - Tolentino
January 25, 2026 AT 04:07Mike P
January 26, 2026 AT 17:47Sarvesh CK
January 27, 2026 AT 18:49Kenji Gaerlan
January 29, 2026 AT 03:28Oren Prettyman
January 29, 2026 AT 15:39Ryan Riesterer
January 31, 2026 AT 05:13