Shared Decision-Making Scripts for Side Effect Trade-Offs in Treatment Choices

Side Effect Trade-Off Calculator
Understand your treatment choices
Your treatment options often come with side effects that impact your daily life. This tool helps you weigh your priorities against potential side effects to make decisions that fit your life.
What matters most to you when considering treatment options?
Select which side effects would be most impactful for your daily life
Personalized Trade-Off Analysis
Your top priority:
Your selected side effects:
How this affects your life
What to discuss with your doctor
When a doctor says, "This medication can cause nausea, fatigue, or dizziness," it’s easy to nod along. But what if nausea means missing work? What if fatigue makes it impossible to play with your kids? What if dizziness increases your risk of falling? These aren’t just side effects-they’re life-altering trade-offs. And too often, patients are left to guess which risks they’re willing to accept. That’s where shared decision-making scripts come in-not as rigid scripts to read from, but as clear, human-centered tools to help you and your clinician weigh what matters most.
Why Side Effect Trade-Offs Are Hard to Talk About
Most people don’t realize how vague medical language can be. When a doctor says a side effect is "rare," they might mean 1 in 100. Or 1 in 1,000. When they say "common," it could be 1 in 5 or 1 in 2. That’s not helpful. And when you’re deciding whether to take a daily pill for the next 10 years, you need to know what you’re signing up for-not just statistically, but personally. A 2021 study in the Journal of General Internal Medicine found that patients who used structured conversations about side effects had 23% less decision regret. Why? Because they weren’t just told what could go wrong-they were asked what they cared about. For example, someone on a statin for cholesterol might be told they have a 15% chance of muscle pain. But if they’re a gardener or a cyclist, that 15% isn’t just a number-it’s a threat to their identity. Someone else might care more about liver changes, even if the risk is lower, because their parent had liver disease. Shared decision-making flips the script: it starts with your life, not the drug label.The SHARE Approach: A Simple Framework for Tough Choices
The Agency for Healthcare Research and Quality (AHRQ) developed the SHARE Approach as a practical five-step model for these conversations. It’s not about memorizing lines-it’s about shifting the rhythm of the visit.- Seek your input. "I want to make sure we pick the best option for you. What are your biggest worries about treatment?" This opens the door. Too often, doctors assume they know what’s important. They don’t.
- Help you explore options. This isn’t just "Option A or B." It’s "Here’s what happens if you take this pill, if you don’t take it, or if you try a different one." Each option comes with its own side effect profile, and each has a different impact on daily life.
- Assess your values. This is where the real work happens. "Some people are okay with mild nausea if it means avoiding hospital visits. Others can’t handle even a little fatigue. Which matters more to you?" The goal isn’t to convince you-it’s to understand you.
- Reach a decision together. Not "I recommend this." Not "You should do this." But "Based on what you’ve told me, this seems like the best fit. Does that match what you’re hoping for?"
- Evaluate your decision. "How are you feeling about this choice now? Are there things we didn’t talk about that are bothering you?" This step is often skipped-but it’s the one that prevents regret down the road.
The Three-Talk Model: Numbers That Stick
The three-talk model, endorsed by the National Institute for Health and Care Excellence (NICE), adds precision to the conversation. It breaks down communication into three clear parts:- Option talk: "There are three ways to manage this. Here’s what each one involves."
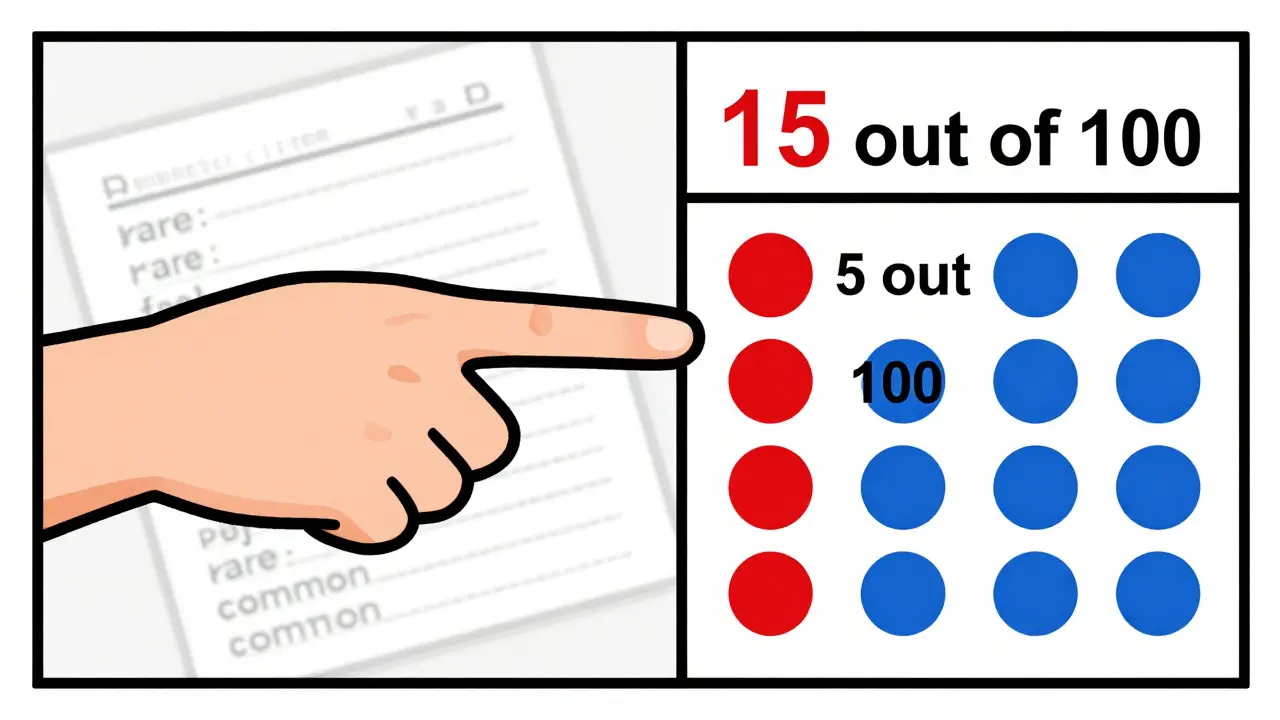
- Decision talk: "Here’s what you might experience. For this medication, 15 out of 100 people get nausea. That means 85 don’t. For the other option, 5 out of 100 get dizziness."
- Support talk: "What’s your threshold? Would 15% nausea be too much? Or is that worth it to avoid the risk of bleeding?"
What Patients Actually Say About Side Effect Decisions
On Reddit’s r/medicine, a patient wrote: "My doctor didn’t just list side effects. She asked, ‘What would make you stop taking this?’ I said, ‘If I can’t hold my granddaughter.’ She said, ‘Then let’s avoid the one that causes extreme fatigue.’ That’s the first time I felt heard." A 2022 survey by the Informed Medical Decisions Foundation found that 84% of patients felt more confident in their choice when clinicians used structured tools to discuss side effects. But here’s the catch: 63% of patients said they felt frustrated when doctors read from scripts without adapting to their situation. That’s the difference between a tool and a performance. The most effective question? "Which side effects would be a deal-breaker for you?" In a 2023 survey, 78% of patients said this single question was the most helpful part of their decision-making process. It’s direct. It’s personal. It doesn’t assume anything.Real-World Impact: When Shared Decision-Making Works
In oncology, where treatment side effects can be severe, the three-talk model has been shown to improve treatment adherence by 78%, according to NICE guidelines. Why? Because patients weren’t just told what to do-they were part of choosing it. For statins, which 86% of patients stop taking because of side effects, Kaiser Permanente rolled out a program with pre-visit videos explaining side effect risks and in-clinic scripts focused on individual tolerance. Result? A 33% drop in discontinuation rates. Even in primary care, where time is tight, clinics that use pre-visit decision aids-like short videos or printed charts-cut consultation time by over 3 minutes. That’s not lost time. It’s time saved later. Patients who make informed decisions have 22% fewer follow-up visits for side effect complaints.What Doesn’t Work
Shared decision-making fails when it becomes a checklist. If a clinician rushes through the steps like a script on autopilot, patients notice. A 2022 study in the Journal of Patient Experience found that rigid use of scripts lowered satisfaction by 19%. People want authenticity, not automation. It also doesn’t work in emergencies. When someone’s having a heart attack, there’s no time for a 10-minute conversation about side effects. But for chronic conditions-diabetes, high blood pressure, depression, cholesterol, arthritis-this is exactly where it shines. And it’s not just about drugs. It’s about procedures, monitoring schedules, lifestyle changes. If a treatment changes how you live, you deserve a say in whether it’s worth it.
How to Get Started
You don’t need to be a doctor to use these tools. Here’s what you can do:- Before your appointment, write down: What’s your biggest fear about treatment? What’s your top priority? (e.g., energy, independence, sleep, avoiding needles)
- Ask: "What are the three options for this? What side effects can I expect with each?"
- Ask: "Which side effects are most likely to affect my daily life?"
- Ask: "What would make you stop taking this? What would make you keep it?"
- Ask: "Can we write down what we agree on?"
The Future Is Here
By 2026, 92% of major U.S. health systems are expected to use shared decision-making tools routinely. Medicare now requires documentation of these conversations for high-risk medications. Electronic health records like Epic include built-in scripts for common conditions like high cholesterol, depression, and anticoagulants. And new tools are emerging. AI systems are being trained to listen to patient-clinician conversations and flag unspoken concerns-like when someone says "I’m fine" but their voice cracks. These aren’t replacements for human connection. They’re amplifiers. The goal isn’t perfect consent. It’s personalized consent. It’s knowing that your choice wasn’t made in a vacuum, but in partnership-with your values, your life, and your fears taken seriously.What to Remember
- Side effects aren’t just numbers-they’re lived experiences. - Your preferences matter more than statistics. - The best decision isn’t the one with the fewest side effects-it’s the one that fits your life. - You have the right to ask: "What would you do if this were your parent?" - Shared decision-making isn’t a script. It’s a conversation you’re allowed to lead.What is shared decision-making for side effects?
Shared decision-making for side effects is a communication process where you and your clinician work together to choose a treatment based on your personal values, concerns, and lifestyle-not just medical facts. It includes discussing the likelihood of side effects, how they might affect your daily life, and what trade-offs you’re willing to accept.
Why are absolute risk numbers better than vague terms like "rare" or "common"?
Vague terms like "rare" or "common" mean different things to different people. Saying "15 out of 100 people get nausea" gives you a clear picture: 15 people in a group of 100 will feel sick, 85 won’t. Research shows this improves patient understanding by 37% compared to vague language, helping you make a more accurate decision.
What’s the most important question to ask about side effects?
"Which side effects would be a deal-breaker for you?" This question cuts through medical jargon and gets to the heart of what matters to you personally. Whether it’s fatigue, weight gain, or memory issues, naming your deal-breakers helps your doctor find the best fit for your life.
Do I need to use a decision aid or app?
Not necessarily, but they help. Simple tools like printed charts, short videos, or even a list of side effects with numbers can make conversations clearer. Many clinics offer these before your visit. If yours doesn’t, ask if they have any resources. You can also find trusted ones online from AHRQ or the Informed Medical Decisions Foundation.
What if my doctor says they don’t have time for this?
You can still start the conversation. Say: "I know you’re busy, but I’d really appreciate just five minutes to talk through what matters most to me about this treatment. It’ll help me stick with it." Studies show patients who do this have fewer follow-up visits, which actually saves time in the long run.
Is shared decision-making only for medications?
No. It applies to any treatment with trade-offs: surgeries, physical therapy, lifestyle changes, monitoring schedules, or even whether to test for a condition. If the choice affects your daily life, you deserve a voice in it.
Haley Parizo
January 4, 2026 AT 09:06This isn't just about meds-it's about power. Doctors hold the keys to your body, and 'rare' or 'common' is just bureaucratic gaslighting. I've been told 'side effects are rare' while my cousin died from a 'rare' reaction. Numbers don't lie, but language does. If you're not telling me 15 out of 100 get nausea, you're not treating me like a person-you're treating me like a data point. And that's not healthcare. That's corporate triage dressed in a white coat.
They want us to 'partner' in decisions? Fine. But first, stop pretending your script is neutral. It's not. It's a tool to make you feel less guilty about rushing through 20 patients an hour. I want the truth, not a TED Talk with a clipboard.
I don't need a checklist. I need a human who's willing to sit in the discomfort with me. Who says, 'I don't know what you'll choose, but I'll help you see it clearly.' That's the only script that matters.
And if your EHR has a checkbox for 'shared decision-making completed,' you're doing it wrong. You're not healing. You're auditing.
Stop making patients do the emotional labor of demanding to be heard. Do your damn job. We're not asking for miracles. We're asking for honesty.
Ian Detrick
January 5, 2026 AT 04:54Man, I wish I'd had this when I was on statins. I thought muscle pain was just 'getting old.' Turns out, it was the drug. I stopped cold turkey, felt like a new person, but spent months feeling like a dumbass for not asking the right questions.
That 'deal-breaker' question? Game-changer. I started using it with my dad when they wanted to put him on blood pressure meds. He said, 'If I can't walk to the store without feeling like I'm dragging a truck, I'm not taking it.' We found a lower-dose option that let him keep his Sunday hikes. That’s the stuff that actually saves lives-not another pill.
Also, the three-talk model? That’s just good communication. Why is this even a 'model'? It should be standard. Like washing your hands before surgery. Basic human decency.
Angela Fisher
January 6, 2026 AT 18:42Okay, but what if this is all a BIG PHARMA scam? 🤔
They want you to think you're 'in control' so you'll take the pills without asking why they cost $400 a month. They give you 'numbers' to make you feel smart-but those numbers are cooked. Who even calculates them? A lab in Switzerland? A guy in a basement in Ohio? 😏
And don't get me started on Epic EHR. That software is owned by a company that also makes vaccines. Coincidence? I think not.
They're training you to ask 'What's your deal-breaker?' so you'll blame yourself when the side effects hit. 'Oh, I should've said NO to fatigue.' No, sweetie. You were manipulated. The system wants you docile, compliant, and medicated. This 'script' is just the velvet glove on the iron fist. 💊👁️
Next they'll make you sign a waiver saying you 'chose' to have your kidneys fail. Don't fall for it. Demand the raw data. Not the sanitized, AHRQ-approved version. I'm not your patient. I'm a citizen.
Liam Tanner
January 7, 2026 AT 18:05I’m a nurse in a rural clinic, and I can tell you-this works. Not because of the script, but because it gives us a structure to actually listen.
One woman came in for hypertension. Said she didn’t care about numbers, just that she could play with her grandkids. We switched her meds. She cried. Said no one had ever asked her what mattered. We didn’t even need a fancy tool. Just a pause. A breath. A question.
Yeah, some docs rush. But most of us? We want this. We’re just tired. Underpaid. Overworked. Give us time. Give us training. And stop calling it a 'script.' It’s a conversation. A real one.
And if you’re a patient reading this? Bring your list. Ask your question. Even if they sigh. Even if they’re late. You’re not being difficult. You’re being human. And that’s the most radical thing you can do.
Palesa Makuru
January 8, 2026 AT 01:52Oh, this is so... American. 🙄
You people treat medicine like a customer service survey. 'What’s your deal-breaker?' Like we’re choosing between Netflix plans. In South Africa, we don’t have the luxury of 'options.' If you get a prescription, you take it. No matter the side effects. Because if you don’t, you die. No one asks you if you can 'hold your granddaughter'-they just hand you the pill and say, 'Live.'
This 'shared decision-making' is a privilege. A luxury for people who have time, insurance, and the education to argue with their doctor. I’ve seen mothers choose between feeding their kids and buying meds. No scripts help there.
Stop romanticizing this. It’s not empowerment. It’s performative healthcare for the middle class. The rest of us just survive.
veronica guillen giles
January 8, 2026 AT 03:38Wow. So now we’re supposed to be our own doctors? Let me guess-next they’ll ask us to read the MRI results ourselves and tell the radiologist if the tumor looks 'suspicious enough.' 😒
Look, I get it. You want to feel empowered. But medicine isn’t a TikTok poll. It’s science. And science doesn’t care what your 'deal-breaker' is. If your cholesterol is 280, it doesn’t matter if you're a yoga instructor or a rock climber-you’re at risk.
Doctors aren’t robots. They’re tired humans who’ve spent 12 years in school trying to save lives, not play therapist. And now you want them to recite a script while you decide whether nausea is 'worth it' because you 'like gardening'? I’m sorry, but I’d rather have a doctor who knows what they’re doing than one who’s just trying to make you feel heard.
Emotional labor is not a substitute for expertise. And no, I don’t want to be your 'partner.' I want you to be my expert.
Vincent Sunio
January 10, 2026 AT 01:57While the intent behind this framework is laudable, its implementation is fraught with epistemological and pragmatic deficiencies. The so-called 'three-talk model' presupposes a Cartesian dichotomy between objective medical facts and subjective patient values, thereby reifying a false binary. Medical risk is not reducible to absolute frequencies; the 15/100 statistic is contingent upon cohort demographics, comorbidities, and pharmacogenetic variance-all of which are omitted in the pedagogical simplification.
Furthermore, the assertion that 'numbers stick' is empirically dubious. Cognitive load theory demonstrates that laypersons misinterpret absolute risk when presented without baseline context (e.g., 15 out of 100 compared to what?). The AHRQ model, while structured, is not evidence-based in its efficacy for long-term adherence-it is, at best, a heuristic for medico-legal compliance.
And to suggest that clinicians are 'not trained' is an indictment of medical education, not a solution. The solution is not more scripts, but better training in probabilistic reasoning and narrative medicine. This is not empowerment. It is commodification of discourse under the guise of patient-centered care.
JUNE OHM
January 11, 2026 AT 01:03OKAY BUT WHAT IF THE DOCTOR IS A ROBOT? 🤖💔
I went to a clinic last year and the doctor just stared at a screen and said '15% chance of nausea' like a vending machine. Then she clicked 'shared decision-making completed' and left. No eye contact. No 'how are you really feeling?' Just a checkbox.
And now they're teaching this to doctors like it's a magic spell? 😭
It’s not about the script. It’s about the soul. If your doctor doesn’t care if you cry when you talk about your grandkids, no amount of 'what’s your deal-breaker?' is gonna fix that.
Also, Epic EHR? That’s the same system that leaked 40 million records in 2021. Are you sure you want to trust your life to a software company that makes more money off your data than your doctor does off your co-pay? 🤔
They’re not giving you power. They’re giving you a form to fill out before they sell you to the insurance company. 💸
Philip Leth
January 12, 2026 AT 22:03My uncle had a stroke. They gave him a pill that made him feel like he was drunk all day. He didn’t say anything because he didn’t want to be 'difficult.'
Then my aunt found this article and asked him: 'What’s one thing you’d give up to feel normal again?' He said, 'I want to sit on the porch and watch the birds.' So they switched his meds. He’s been outside every morning since.
That’s all this is. Not a script. Not a checklist. Just someone asking, 'What’s your life worth?'
Doctors aren’t gods. We’re not patients. We’re people. And we deserve to be treated like it.
So ask. Even if they sigh. Even if they’re busy. You’re not being annoying. You’re being alive.
Shanahan Crowell
January 13, 2026 AT 06:04I’m a cancer survivor. I’ve been through chemo, radiation, and a dozen different meds. And the one thing that saved me? Not the science. Not the stats. The moment my oncologist looked me in the eye and said, 'If you can’t sleep, if you can’t laugh, if you can’t hug your wife-then this isn’t working. Let’s try something else.'
That wasn’t a script. That was a human.
So if you’re a patient: don’t wait for them to ask. Ask first. 'What’s the worst thing this could do to my life?'
If they hesitate? That’s your answer.
If they know? That’s your doctor.
And if you’re a clinician? Don’t just check the box. Look up. Listen. Breathe.
This isn’t about protocols.
This is about love.
And love doesn’t need a form.
It just needs presence.
Kerry Howarth
January 14, 2026 AT 10:08Ask: 'What would make you stop?'
Then listen.
Don’t interrupt.
Don’t fix.
Just sit with it.
That’s all it takes.