Slow Up-Titration Schedules: How Gradual Dose Increases Help You Tolerate Medication Side Effects
Titration Schedule Calculator
Choose Your Medication
Key Notes
Slow titration helps your body adapt safely. Pushing through symptoms can lead to treatment discontinuation.
Why Starting Low and Going Slow Works Better Than Jumping to Full Dose
Imagine starting a new medication and feeling sick within days-nausea, dizziness, fatigue. You stop taking it. That’s not failure. It’s often the result of being given too much, too fast. Slow up-titration isn’t just a medical term; it’s a practical, proven way to help your body adjust to powerful drugs without overwhelming it. Instead of jumping straight to the full dose, you start with a tiny amount and increase it slowly over weeks or even months. This approach isn’t about being cautious-it’s about working with your body, not against it.
The science behind this is clear. In heart failure, patients who started on full doses of beta-blockers like metoprolol had an 88% failure rate in sticking with the treatment. But when doctors began at 6.25mg twice daily and slowly increased over six weeks, 83% of patients stayed on track. That’s not luck. It’s physiology. Your receptors need time to adapt. Your gut needs time to settle. Your blood pressure needs time to stabilize.
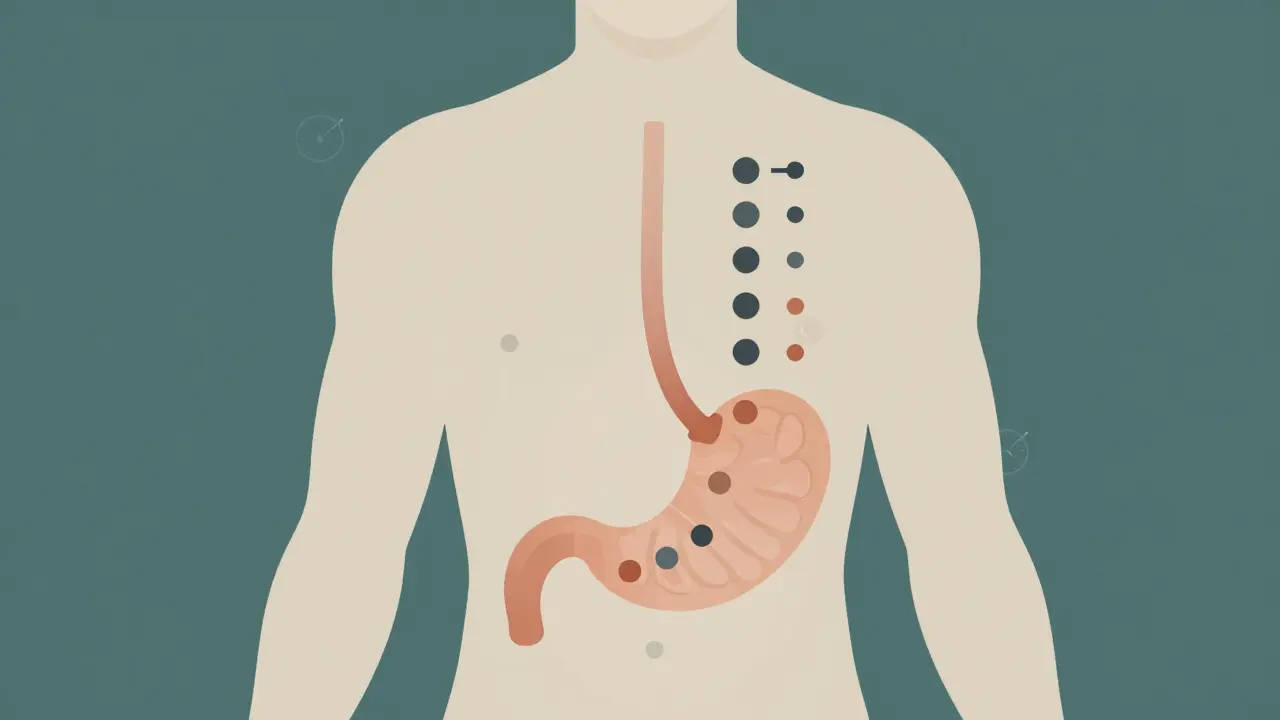
How Slow Up-Titration Actually Works in Your Body
When you take a new drug like a GLP-1 receptor agonist (think semaglutide for diabetes or weight loss), it hits your system hard. At full dose, up to 65% of people get severe nausea. But if you start at 0.25mg once a week for four weeks, your body begins to adjust. The receptors in your brain and gut that trigger nausea slowly become less sensitive. By the time you reach 0.5mg, your stomach isn’t screaming anymore. By 1.0mg, you barely notice it. That’s tolerance-not because you’re tough, but because your biology changed.
This isn’t unique to GLP-1 drugs. Beta-blockers, ACE inhibitors, and even some antidepressants follow the same pattern. Rapid dosing causes sudden drops in heart rate or blood pressure. Slow titration lets your cardiovascular system recalibrate. A 2019 analysis of the PARADIGM-HF trial showed that patients on structured titration schedules had 52% fewer severe side effects than those rushed into full doses. That’s not a small difference-it’s the difference between staying on treatment and quitting it.
Real-World Titration Schedules You Need to Know
Not all medications titrate the same way. The timeline depends on the drug, its side effects, and how your body processes it. Here’s what you’re likely to see:
- Oral semaglutide (Rybelsus): Start at 3mg daily for 30 days, then increase to 7mg for another 30 days. After that, you may go to 14mg. Total time to max dose: about 60 days.
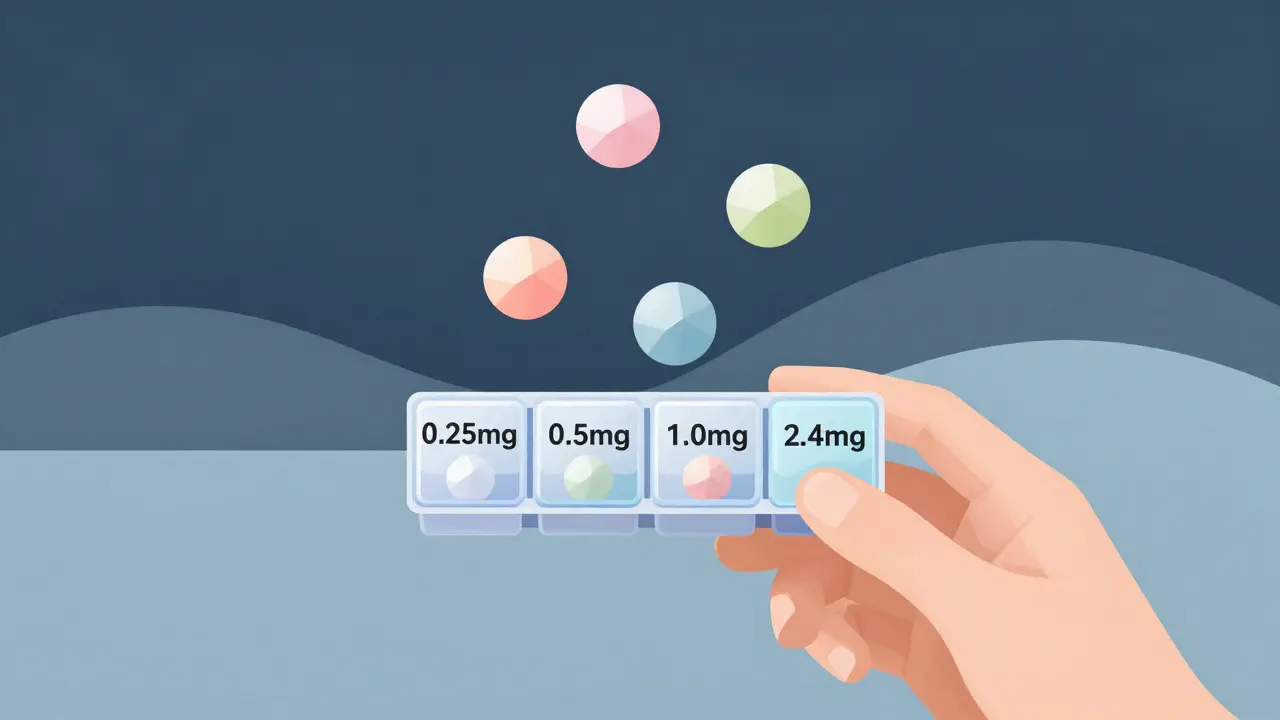
- Subcutaneous semaglutide (Wegovy, Ozempic): Begin at 0.25mg once a week for four weeks. Then 0.5mg for four weeks, then 1.0mg for at least four weeks. For weight loss, you might eventually reach 2.4mg-after 16 to 20 weeks.
- Metoprolol (for heart failure): Start at 6.25mg twice daily. Double the dose every two to four weeks, as long as your blood pressure and heart rate stay stable. Full dose may take 8 to 12 weeks.
- Enalapril (ACE inhibitor): Begin at 2.5mg once daily. Increase by 2.5mg every 1-2 weeks until reaching 10-20mg daily.
These aren’t arbitrary. They’re based on clinical trials that tracked side effects at each step. The FDA and major medical societies like the American Heart Association and American Diabetes Association have standardized these schedules because they work.
Why Some People Still Struggle-Even With Slow Titration
Slow up-titration helps most people, but it’s not magic. A 2021 study found that 22% of patients over 65 had trouble keeping up with changing doses. Why? The schedules are complex. A pill that’s 3mg one month becomes 7mg the next. You might need to switch from tablets to liquids. You have to remember when to call your doctor for the next increase.
One patient on Reddit, u/GLP1Survivor, shared: “I tried skipping the first step with my first GLP-1. I threw up for three days straight. I quit. When I did it right-starting low-I made it to 2.4mg without a single day of nausea.” That’s the pattern. People who rush fail. People who follow the schedule succeed.
Another issue: side effects that linger. The “2-week rule” is key. If nausea or dizziness lasts more than two weeks at a given dose, don’t just push through. Contact your provider. You might need to stay at that dose longer, or your medication might need adjustment. Pushing through isn’t bravery-it’s risky.
Tools and Tips to Stay on Track
Sticking to a titration schedule takes effort. Here’s how to make it easier:
- Use a pill organizer with dates. Label each compartment for the week and dose. Don’t rely on memory.
- Set phone reminders. Apps like Medisafe or MyTherapy send alerts for dose changes and doctor visits. Studies show they improve adherence by 18%.
- Keep a side effect journal. Note when nausea starts, how bad it is, and what you ate. This helps your doctor decide if you’re ready for the next step.
- Ask for a printed schedule. Many manufacturers offer clear, simple charts. If yours doesn’t, ask your pharmacist to make one.
Some clinics now use digital tools like Omada Health’s GLP-1 program, which sends weekly check-ins and adjusts titration based on how you’re feeling. In a 2023 pilot, these tools cut side effect-related dropouts by 41%. That’s huge.
When Slow Titration Isn’t the Right Choice
Slow up-titration is ideal for chronic conditions where long-term safety matters: heart failure, type 2 diabetes, hypertension. But it’s not for emergencies. If you’re having a hypertensive crisis, you don’t wait weeks to get your blood pressure down. You need labetalol or nitroprusside-fast-acting drugs that work immediately.
Even in chronic cases, some drugs don’t need slow titration. SGLT2 inhibitors like Jardiance or Farxiga are often started at full dose because they’re well-tolerated from day one. A 2023 trial (DIAMOND) showed no extra benefit from titrating them slowly. For metformin, the American College of Endocrinology says rapid escalation is fine for patients with HbA1c over 9%-as long as they’re monitored.
Slow titration is a tool, not a rule. The goal isn’t to drag things out. It’s to get you to the right dose safely, without quitting.
What Success Looks Like
One 68-year-old man with severe heart failure was Class III-unable to walk across a room without stopping. He started on a slow titration schedule for four medications: an ACE inhibitor, beta-blocker, MRA, and SGLT2 inhibitor. He had weekly telehealth visits. He kept a journal. He didn’t skip a single dose change. Five months later, he was Class I. He could walk his dog, climb stairs, sleep through the night. He didn’t feel better because the drugs were stronger. He felt better because his body had time to adapt.
That’s the real win. It’s not about how fast you get to the target dose. It’s about whether you stay on the treatment long enough to benefit from it. Slow up-titration isn’t about patience. It’s about persistence. And the data shows: patients who stick with it live longer, feel better, and avoid hospitalizations.
What to Do Next
If you’re starting a new medication that requires titration:
- Ask your doctor for the full schedule in writing.
- Set reminders for each dose change.
- Know the warning signs: if side effects last more than two weeks, call your provider.
- Don’t compare your pace to someone else’s. Your body adapts differently.
- Celebrate small wins. Making it through week 4 at 0.25mg? That’s a victory.
Slow up-titration isn’t a delay. It’s a strategy. It’s how modern medicine keeps you alive without making you miserable.
How long does it usually take to reach the full dose with slow up-titration?
It varies by medication. For GLP-1 agonists like semaglutide, it can take 16 to 20 weeks to reach the highest dose. For beta-blockers in heart failure, it’s often 8 to 12 weeks. Some drugs, like SGLT2 inhibitors, don’t require titration at all. Always follow your provider’s schedule-it’s tailored to your drug and condition.
What if I miss a dose during titration?
Don’t double up. If you miss a dose at your current level, take it as soon as you remember-if it’s still the same day. If it’s the next day, skip it and wait until your next scheduled dose. Never jump ahead to the next level early. Contact your provider if you miss more than two doses in a row. They may delay your next increase.
Can I speed up the titration if I feel fine?
No. Feeling fine doesn’t mean your body is ready. Side effects can build up quietly-like slight drops in kidney function or low blood pressure that you don’t notice. Your provider schedules increases based on safety data, not how you feel on a given day. Rushing increases your risk of serious side effects and treatment failure.
Why do some medications need slow titration and others don’t?
It depends on how the drug affects your body. GLP-1 agonists cause strong nausea because they slow digestion-your gut needs time to adjust. Beta-blockers lower heart rate suddenly, which can cause dizziness. Drugs like metformin or SGLT2 inhibitors have gentler side effects and are safer at full dose from the start. The decision is based on decades of clinical research.
Is slow titration covered by insurance?
Yes. Insurance covers the medications and the visits needed for titration. Many insurers now require structured titration for certain drugs to reduce long-term costs from hospitalizations and treatment discontinuation. If your provider recommends a titration schedule, your insurance should support it through regular check-ups and follow-ups.
Nancy Kou
December 19, 2025 AT 18:39Matt Davies
December 20, 2025 AT 08:16mark shortus
December 20, 2025 AT 08:56Vicki Belcher
December 20, 2025 AT 19:55Hussien SLeiman
December 22, 2025 AT 09:01Nicole Rutherford
December 23, 2025 AT 23:11Jedidiah Massey
December 25, 2025 AT 10:03Allison Pannabekcer
December 27, 2025 AT 07:10Marsha Jentzsch
December 27, 2025 AT 18:50Emily P
December 29, 2025 AT 11:34Ashley Bliss
December 31, 2025 AT 10:07