Statins in Women: What You Need to Know About Sex-Specific Side Effects

Statin Side Effect Risk Calculator
This tool helps you assess your personal risk of statin side effects based on key factors highlighted in the article. Results are for informational purposes only and should not replace medical advice.
Statins save lives. They lower bad cholesterol, reduce heart attacks, and prevent strokes - especially in people at high risk. But for women, taking statins isn’t always as straightforward as it is for men. While these drugs work just as well at preventing heart disease in women, the side effects? They’re different. And often, they’re worse.
Women Get Muscle Pain More Often - And It’s Not Just in Their Heads
If you’re a woman taking a statin and you’ve felt sore, weak, or achy in your muscles, you’re not alone. In fact, you’re more likely than a man to feel it. The USAGE survey, which tracked over 10,000 statin users, found that 31% of women reported new or worsening muscle pain, compared to just 26% of men. That difference isn’t small. It’s statistically significant. And it leads to real consequences: women are more likely to stop taking their statins because of it. Why does this happen? It’s not about being "overly sensitive." It’s biology. Women generally have lower kidney function after adjusting for body size - about 15-20% lower glomerular filtration rates than men. That means statins stick around longer in the bloodstream. Women also tend to have higher body fat percentages - around 25-30% on average versus 15-20% in men. Since statins are fat-soluble, they get stored in fat tissue and released slowly, increasing exposure over time. This is especially true for women over 65. Older women are 1.5 to 2 times more likely to develop statin-induced myopathy than older men. Why? On top of slower kidney clearance, they’re more likely to be taking multiple medications - like blood pressure pills or blood thinners - that interact with statins. Simvastatin, for example, becomes dangerously toxic when mixed with common calcium channel blockers, increasing the risk of muscle damage by 300%.Statins Can Raise Your Risk of Diabetes - Especially After Menopause
You might have heard statins can increase the risk of type 2 diabetes. That’s true. But for women, especially after menopause, that risk isn’t just a side note - it’s a real concern. The FDA added a warning about this in 2012. Since then, studies have shown statins raise diabetes risk by 9% to 27%, depending on the drug and how long you take it. The JUPITER trial found rosuvastatin increased diabetes risk by 27% over two years. A 2013 study in the Journal of the American College of Cardiology looked specifically at post-menopausal women and found that any statin - no matter the dose or type - could raise diabetes risk after three years of use. The good news? The heart benefits still outweigh the diabetes risk for most women who need statins. But here’s the catch: if you’re a woman over 50, your doctor should be checking your fasting blood sugar every 3 to 6 months after you start the medication. It’s not optional. It’s essential. And if your glucose levels start creeping up, switching to a different statin or adding ezetimibe might be a smarter move than pushing through with a higher dose.Doctors Don’t Always Explain the Risks - And Women Notice
Here’s something no one talks about enough: communication gaps. In a 2019 study of nearly 5,700 patients, women were 34% more likely than men to say their doctor never explained how high cholesterol leads to heart disease. Nearly half of women reported never getting a clear picture of why they needed a statin - compared to just over 30% of men. That lack of explanation matters. When people don’t understand why they’re taking a drug, they’re more likely to quit when side effects show up. And women? They’re 2.3 times more likely than men to try three or more different statins before finding one they can tolerate. Yet, when statins don’t work, women are 37% less likely to be offered alternatives like ezetimibe or PCSK9 inhibitors. This isn’t about patients being difficult. It’s about bias. Studies show doctors are more likely to dismiss muscle pain complaints from women as "non-specific" or "psychological." But the data doesn’t lie - women’s bodies process these drugs differently. When a woman says her legs feel heavy or she can’t climb stairs like she used to, it’s not in her head. It’s in her muscles.Adherence Is Lower - And It’s Not Just About Cost
At 12 months, only 63% of women are still taking their statin. For men? It’s 77%. That’s an 18.7% drop-off - and it’s not because women don’t care about their health. It’s because of a mix of factors: side effects, poor communication, and yes - cost. Women are more likely to prioritize family healthcare over their own. If they’re paying for their child’s asthma inhaler, their partner’s blood pressure meds, and their own statin, something’s got to give. In one study, 29% of women cited cost as the reason they skipped doses, compared to 19% of men. But even when cost isn’t an issue, adherence stays lower. Why? Because the side effects aren’t being managed well.What About Younger Women? Pregnancy and Contraception Matter
If you’re a woman of childbearing age, statins are a hard no during pregnancy. The FDA classifies all statins as Pregnancy Category X - meaning they can cause serious birth defects. That’s not a theoretical risk. Animal studies show clear harm. Yet, a 2022 expert guideline found that 15% of statin prescriptions for women aged 18 to 45 had no documented discussion about contraception. That’s unacceptable. Before starting a statin, every woman who could get pregnant needs a clear plan: which birth control method are you using? Are you sure it’s reliable? Are you aware of what happens if you miss a pill? Doctors need to ask these questions - and women need to feel safe answering them. No one should be afraid to talk about birth control with their doctor. And no one should be prescribed a statin without that conversation.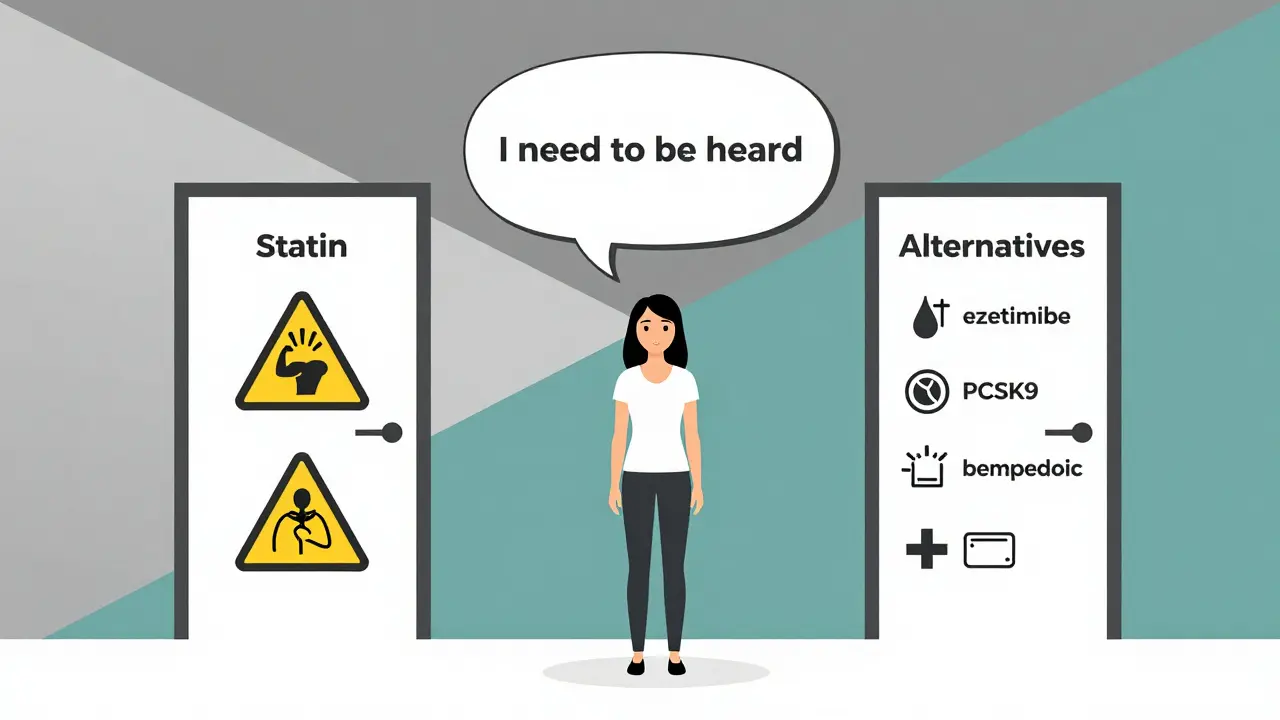
What Can You Do? Practical Steps for Women on Statins
If you’re a woman taking - or considering - a statin, here’s what actually helps:- Start low, go slow. Instead of jumping to 20 mg of atorvastatin, start at 10 mg. The Dutch STATINWISE trial showed this approach improved adherence by 32% in women.
- Ask about genetic testing. A gene called SLCO1B1 affects how your body handles statins. About 23% of women have a variant that increases muscle damage risk. A simple blood test before starting can help pick the safest statin.
- Track your symptoms. Keep a simple log: when did the muscle pain start? Did it get worse after a dose change? Did it go away after skipping a few days? Bring this to your doctor.
- Ask for alternatives. If statins don’t work, don’t accept "just try another one" as the only option. Ezetimibe, bempedoic acid, and PCSK9 inhibitors are effective, non-statin options. They’re not always covered, but they’re worth fighting for.
- Get your blood sugar checked. If you’re over 50, ask for a fasting glucose test every 6 months. Early detection of prediabetes can change your treatment plan before it becomes diabetes.
It’s Not About Fear - It’s About Smart Choices
Statins aren’t perfect. But for women at risk of heart disease, they’re still one of the most powerful tools we have. The problem isn’t the drug. It’s how we’ve been using it - with a one-size-fits-all approach that ignores biology, communication, and context. The good news? We’re starting to fix it. New guidelines, better training for doctors, and patient tools like the "Statin Choice" decision aid - shown in a 2021 study to reduce discontinuation by 40% - are making a difference. If you’re a woman on statins, you deserve to be heard. You deserve to understand why you’re taking it. And you deserve a treatment plan that fits your body - not just the textbook.Do statins cause more side effects in women than in men?
Yes. Women are more likely to experience muscle pain, weakness, and fatigue from statins. Studies show 31% of women report muscle symptoms compared to 26% of men. Women also have higher rates of statin discontinuation due to side effects, partly because of biological differences in how their bodies process the drugs - including lower kidney function and higher body fat percentages.
Can statins cause diabetes in women?
Yes. Statins increase the risk of developing type 2 diabetes by 9% to 27%, depending on the type and duration of use. This risk is especially notable in post-menopausal women, where studies show any statin - regardless of dose - can raise diabetes risk after three years. Regular fasting blood sugar checks every 3 to 6 months are recommended for women over 50 on statins.
Why are women less likely to be prescribed statins even when they need them?
Historically, women were underrepresented in clinical trials, leading to uncertainty about benefits and risks. Even today, doctors may underestimate women’s cardiovascular risk or dismiss their side effect reports as "atypical." As a result, women are 11% less likely than men to receive statins after meeting guideline criteria - even after a heart attack.
Should women take a lower dose of statins?
Often, yes. Starting with a lower dose - like atorvastatin 10 mg instead of 20 mg - reduces side effects and improves adherence. The Dutch STATINWISE trial found this approach increased long-term use by 32% in women. Lower doses are just as effective for many women, especially those who are older, smaller, or taking other medications.
What should I do if I can’t tolerate statins?
Don’t stop without talking to your doctor. There are non-statin options like ezetimibe, bempedoic acid, and PCSK9 inhibitors that lower LDL cholesterol effectively. These are especially useful for women with statin intolerance. Genetic testing for SLCO1B1 variants can also help identify which statin - if any - might work best for you.
Are statins safe during menopause?
Statins are still recommended for women during menopause who are at high risk for heart disease - because estrogen loss speeds up artery damage. However, muscle side effects become more common after menopause, affecting 41% of post-menopausal women versus 33% of pre-menopausal women. Careful dosing, monitoring, and checking for drug interactions are critical during this time.
Can statins affect my mental health or cause brain fog?
Some women report memory issues or brain fog, but large studies haven’t found a clear link between statins and cognitive decline. The FDA reviewed data and concluded there’s no consistent evidence statins cause dementia or memory loss. If you notice changes, track them and discuss them with your doctor - but don’t assume it’s the statin without ruling out other causes like sleep, stress, or hormones.
How do I know if I really need a statin?
Your need depends on your overall risk - not just your cholesterol number. Factors like age, blood pressure, smoking, diabetes, family history, and CAC score (coronary calcium scan) matter more. For women, especially those over 55, even a modestly elevated LDL can signal high risk. Use tools like the American Heart Association’s risk calculator and ask your doctor to explain your 10-year risk in plain terms.
Annette Robinson
January 7, 2026 AT 22:50I’ve been on atorvastatin for three years, and honestly? The muscle fatigue was brutal. I thought I was just getting older until I read this. Started at 10mg instead of 20 - life changed. My knees don’t feel like concrete anymore. If you’re a woman and your doctor pushes a high dose right away, push back. You’re not being difficult - you’re being smart.
Also, tracking symptoms in a notes app? Game changer. I showed my doc the log - he actually listened. Who knew?
Aubrey Mallory
January 9, 2026 AT 10:28Let’s be real - medicine was designed by men for men. Women’s pain is dismissed as ‘hormonal’ or ‘stress-related’ until it’s too late. Statin myopathy isn’t ‘in your head’ - it’s in your mitochondria. And if your doctor doesn’t know that, find a new one. This isn’t opinion. It’s pharmacokinetics.
Stop accepting ‘try another statin’ as an answer. Ask for SLCO1B1 testing. Demand it. Your body deserves better than trial-and-error guesswork.
christy lianto
January 9, 2026 AT 15:28As a 58-year-old woman who just got off simvastatin after 18 months of leg pain that made walking to the mailbox feel like climbing a mountain - I’m screaming this from the rooftops: START LOW.
I was on 40mg. My doctor said ‘it’s fine, you’re just sensitive.’ I switched to 10mg atorvastatin. Muscle pain? Gone. LDL? Still under control. Why is this not standard practice? Because we’ve been trained to suffer quietly.
Also - get your blood sugar checked every 6 months. I didn’t. Now I’m prediabetic. Don’t make my mistake.
Lois Li
January 10, 2026 AT 05:53I think this article is really important but i think we need to talk about the cost issue more. i know women who skip doses because they have to choose between their statin and their kids’ insulin. its not laziness. its survival. and no one talks about that. doctors focus on side effects but dont ask if you can even afford the pill.
also, if you’re on medicaid or uninsured, good luck getting ezetimibe. it’s like asking for a unicorn.
Manish Kumar
January 12, 2026 AT 01:56There’s an underlying metaphysical truth here: modern medicine treats the body as a machine, ignoring the subtle, feminine rhythms of biological variation. Statins are not neutral agents - they interact with hormonal landscapes, fat distribution, renal flow - all of which are inherently gendered. To treat a woman as if she were a man with a uterus is not just negligent - it’s ontologically flawed.
We must move beyond the Cartesian model of health. The body is not a clock. It is a symphony - and women’s bodies play in a different key. To ignore that is not science. It is dogma dressed in lab coats.
And yet, the system resists. Because change threatens power. And power prefers uniformity over truth.
Dave Old-Wolf
January 13, 2026 AT 04:57I’m a guy, but my mom’s on a statin and she was having serious leg cramps. She didn’t tell anyone for months because she didn’t want to be a ‘complainer.’ When she finally did, her doc just upped the dose. She cried in my car after that appointment.
This article? I printed it out and gave it to her. She’s now on 10mg atorvastatin. No more cramps. And she got her glucose checked - prediabetic, but caught early. She’s doing yoga now. Life’s better.
Thanks for writing this. My mom says you’re a hero.
Prakash Sharma
January 14, 2026 AT 01:48Why are we even talking about this? In India, women don’t even get cholesterol tests unless they’re 60+. Here you’re debating doses and genes - while half the world doesn’t have access to basic meds. This is elite first-world navel-gazing.
Statins are expensive. Doctors are overworked. Women don’t complain because they’re busy keeping families alive. Stop making this about identity politics. Fix healthcare for everyone - not just the ones who can afford to blog about it.
Donny Airlangga
January 15, 2026 AT 03:48My wife’s on rosuvastatin. She’s 52. Got her glucose checked every 4 months like the article said - and yeah, it crept up. We switched to ezetimibe. Her LDL’s still at 85. No muscle pain. No diabetes.
Doctors act like statins are the only option. They’re not. They’re just the easiest to prescribe. If you’re a woman and you’re struggling - don’t accept ‘just stick with it.’ Ask for alternatives. You’re not being difficult. You’re being proactive.
Molly Silvernale
January 15, 2026 AT 04:03Statins-those little white pills-have become the pharmaceutical equivalent of a velvet rope at a club: everyone’s invited, but only some are told the dress code. Women? We’re told to wear heels. Men? They get sneakers.
And yet-we’re the ones who show up in full makeup, still bleeding from the blisters, smiling politely while our bodies scream. This isn’t compliance. It’s survival. And it’s exhausting.
Someone needs to design a statin that doesn’t treat women like faulty prototypes. Until then? I’m keeping my log. And my voice. Loud. Unapologetic. Un-punctuated. Because I’m tired of punctuation being the only thing that’s ‘correct’ about how I’m treated.
Kristina Felixita
January 15, 2026 AT 17:26My mom’s Indian, she’s 67, and she’s been on a statin since 2018. She never told me she was having muscle pain because she didn’t want to ‘bother’ me. I found out when she fell getting out of the shower.
I took her to a new doctor, showed them this article, and now she’s on 10mg pravastatin. She’s walking again. She’s making her samosas again. And she’s finally talking about her health like it matters.
Also - she started checking her sugar. She’s got a little tracker on her fridge now. We’re proud of her.
Thank you for writing this. I’m sharing it with every auntie I know.
Joanna Brancewicz
January 15, 2026 AT 18:54SLCO1B1 polymorphism prevalence: 23% in women. Statin-induced myopathy: 31% vs 26%. Fasting glucose monitoring: essential post-menopause. Ezetimibe: non-statin, LDL-lowering, 18% reduction. PCSK9i: 60%+ reduction, cost barrier. Adherence: 63% women vs 77% men. Documentation gap: 34% less explained to women. All evidence-based. No speculation. Just data.
Stop gaslighting. Start prescribing wisely.
Evan Smith
January 16, 2026 AT 23:33So let me get this straight - women get more side effects, doctors don’t explain shit, and now we’re supposed to feel bad because we’re not ‘compliant’? Sounds like the system is broken, not the patients.
Also, I’ve got a friend who got her statin prescription while on birth control and no one asked if she was using it properly. That’s not negligence. That’s malpractice with a smile.
Why do we keep pretending this is just about cholesterol? It’s about who gets listened to. And right now? Women are still the afterthought.
Ken Porter
January 17, 2026 AT 22:44Statins are overprescribed. Women are more likely to be on them because they’re easier to treat than lifestyle changes. Meanwhile, real heart health - diet, sleep, stress - gets ignored. This isn’t biology. It’s corporate medicine.
Also, ‘genetic testing’? That’s a $300 add-on most insurers won’t cover. So yeah, nice article. But it’s just a glossy pamphlet for people who can afford to care.
swati Thounaojam
January 18, 2026 AT 06:04i live in india and my mom is on statin. no one ever told her about diabetes risk. she found out by accident when she went for a checkup. now she checks her sugar every week. i wish more doctors here knew this. we need more awareness. thank you for writing this.