Tizanidine and Ciprofloxacin: Why This Drug Combo Can Cause Dangerous Low Blood Pressure and Extreme Drowsiness
Tizanidine & Ciprofloxacin Safety Calculator
This calculator helps determine the safe timeframe for restarting Tizanidine after completing Ciprofloxacin treatment. Due to their dangerous interaction, you must wait at least 5-7 days after your last Ciprofloxacin dose before restarting Tizanidine.
Recommended Restart Window
Why This Timing Matters
Ciprofloxacin inhibits the CYP1A2 enzyme for up to 72 hours after your last dose. This enzyme is the only way your body processes Tizanidine. When blocked, Tizanidine levels can increase 10-33 times higher than normal, causing severe hypotension (blood pressure below 70 mm Hg) and extreme drowsiness. Waiting at least 5-7 days allows the enzyme to fully recover.
Imagine taking a muscle relaxant for a bad back spasm, and then getting prescribed ciprofloxacin for a urinary tract infection. It seems harmless-two common meds, right? But if you take them together, you could suddenly drop your blood pressure to dangerous levels, pass out, or fall into a deep, unresponsive sleep. This isn’t a rare accident. It’s a well-documented, life-threatening interaction that still happens far too often.
How Tizanidine Works-and Why It’s So Fragile
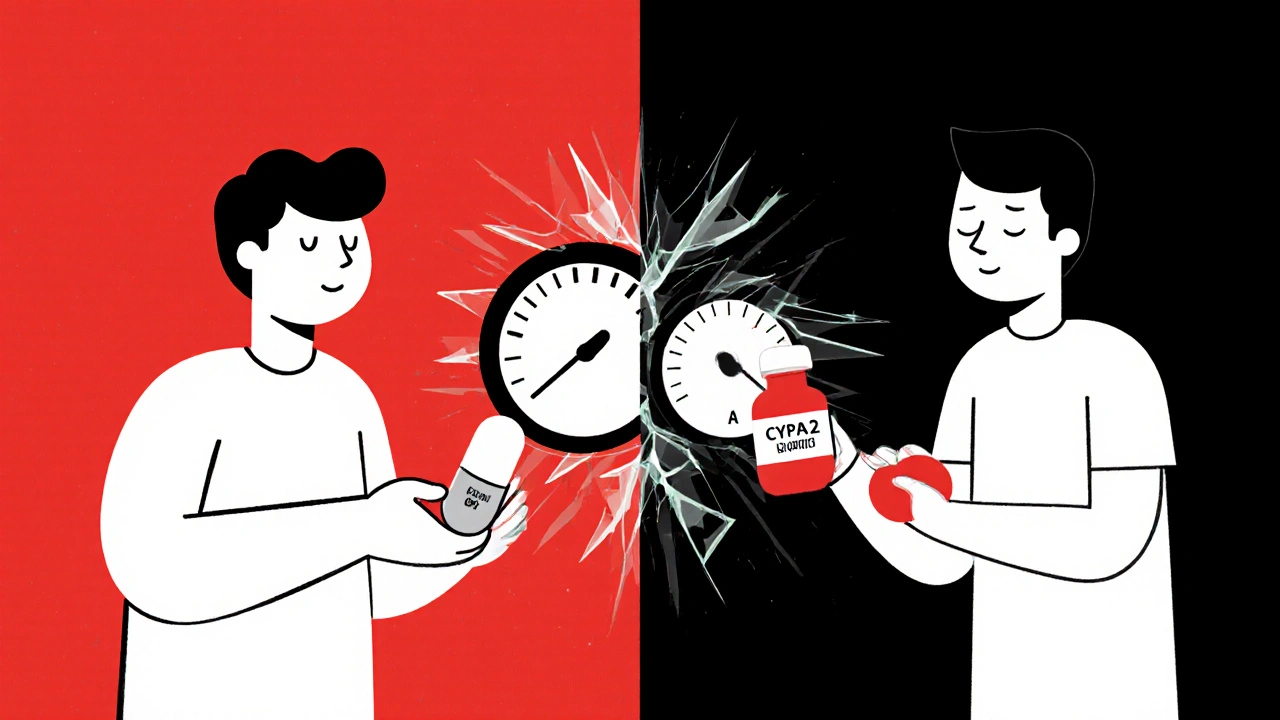
Tizanidine is a muscle relaxant used for short-term relief of muscle spasms and spasticity, often from back pain or conditions like multiple sclerosis. It works by calming overactive nerves in the brain and spinal cord. But here’s the catch: your body breaks down tizanidine using just one enzyme-CYP1A2. Almost 95% of it is cleared this way. That makes tizanidine unusually vulnerable. If something blocks CYP1A2, tizanidine doesn’t get processed. It builds up. Fast.
When tizanidine levels spike, its effects go from helpful to overwhelming. You might feel dizzy. Then your blood pressure plummets. Your limbs feel heavy. You can’t stay awake. In severe cases, systolic blood pressure drops below 70 mm Hg. That’s not just lightheadedness-it’s a medical emergency. Patients have needed IV fluids, vasopressors, and ICU care after this combo.
Ciprofloxacin: The Silent Saboteur
Ciprofloxacin is a fluoroquinolone antibiotic. It’s effective against stubborn infections like UTIs, pneumonia, and sinusitis. But it’s also one of the strongest known inhibitors of CYP1A2. When you take ciprofloxacin, it shuts down the enzyme that clears tizanidine. Clinical studies show this causes tizanidine levels to jump 10 to 33 times higher than normal.
This isn’t theoretical. Researchers at Vanderbilt University Medical Center analyzed real patient records and found a 43% higher risk of severe hypotension when these two drugs were taken together. The effect isn’t delayed-it kicks in within hours. Patients reported extreme drowsiness, confusion, and fainting shortly after taking both meds. One patient, a 68-year-old woman with chronic back pain and a UTI, collapsed at home after taking both pills on the same day. Her blood pressure was 68/42. She spent three days in the hospital.
Why Other Muscle Relaxants Are Safer
Not all muscle relaxants are this risky. Cyclobenzaprine, for example, is metabolized through multiple enzyme pathways-CYP1A2, CYP3A4, CYP2D6. If one gets blocked, others can still clear the drug. That’s why cyclobenzaprine doesn’t cause the same spike in blood pressure when paired with ciprofloxacin.
Studies comparing the two found that tizanidine users had significantly more severe hypotensive events than cyclobenzaprine users on the same antibiotics. The difference isn’t subtle-it’s structural. Tizanidine has no backup metabolic route. One blocker, and it’s a bomb waiting to go off.

Who’s Most at Risk?
This interaction doesn’t hit everyone the same way. Certain patients are walking into danger without knowing it:
- Elderly patients-their livers process drugs slower, so tizanidine lingers even without ciprofloxacin.
- People on multiple blood pressure meds-if you’re already taking three or more antihypertensives, adding tizanidine and ciprofloxacin can crash your pressure.
- Those with kidney or liver disease-both organs help clear these drugs. Damage to either raises the risk.
- Patients on other CYP1A2 inhibitors-fluvoxamine (an antidepressant), amiodarone (a heart drug), or even high-dose oral contraceptives can do the same thing as ciprofloxacin.
These aren’t edge cases. In the Vanderbilt study, over 60% of patients who had this interaction were over 60 and already on antihypertensives. The risk isn’t just higher-it’s predictable.
What Doctors Are Supposed to Do
The FDA and European Medicines Agency both list this combination as absolutely contraindicated. That means: don’t do it. Ever. The tizanidine label warns this clearly. So why does it still happen?
Because doctors are busy. Because patients don’t tell them about every med they’re taking. Because prescriptions are written in different clinics-pain specialist here, urgent care there. Electronic health records often don’t catch it unless they’re programmed to. A 2022 study found that despite clear warnings, this combo was still being prescribed in primary care, orthopedics, and rheumatology clinics across the U.S.
Experts like Dr. Cecilia Chung at Vanderbilt say the solution isn’t just better warnings-it’s better systems. Alerts in e-prescribing software should block this combo outright. Pharmacists should flag it at the counter. Patients need to be told, clearly and repeatedly: Do not take ciprofloxacin if you’re on tizanidine.
What to Do Instead
If you’re on tizanidine and get an infection:
- Don’t take ciprofloxacin. Tell your doctor you’re on tizanidine.
- Ask for a safer antibiotic. Amoxicillin, nitrofurantoin, or doxycycline don’t inhibit CYP1A2. They’re just as effective for most infections.
- If ciprofloxacin is your only option, stop tizanidine completely during the antibiotic course-and wait at least 5 to 7 days after finishing it before restarting tizanidine. Your body needs time to clear the ciprofloxacin before the enzyme can work again.
- Never adjust doses yourself. Even cutting tizanidine in half won’t prevent the interaction. The enzyme blockage is too powerful.
For chronic pain, consider non-drug options during antibiotic treatment: heat therapy, physical therapy, or even short-term use of acetaminophen. Don’t risk your safety for a few extra days of pain relief.
What to Watch For
If you accidentally took both drugs together, watch for these signs within 2-6 hours:
- Sudden dizziness or lightheadedness
- Blurred vision
- Extreme tiredness-so much you can’t stay awake
- Feeling like you might pass out
- Heart beating fast or irregularly
If you experience any of these, sit or lie down immediately. Call 911 or go to the ER. Don’t wait. This isn’t a mild side effect. It’s a medical crisis.
Why This Matters Beyond the Lab
This isn’t just a pharmacology footnote. It’s a real-world safety failure. Tizanidine is prescribed over 7 million times a year in the U.S. Ciprofloxacin is one of the most common antibiotics. Millions of people could be at risk.
The WHO’s global drug safety database, VigiBase, has documented dozens of severe cases-including deaths-linked to this combo. Yet, most patients never hear about it. Their doctors don’t mention it. The system keeps failing them.
Until prescribing systems are forced to block this combo, until pharmacists are trained to question it, until patients are told plainly: Don’t mix these two-people will keep getting hurt.
You don’t need to be a scientist to understand this: if your doctor prescribes ciprofloxacin while you’re on tizanidine, ask: Is this safe? If they hesitate, get a second opinion. Your life isn’t worth the risk.
Can I take tizanidine and ciprofloxacin if I space them out by a few hours?
No. Spacing them out won’t help. Ciprofloxacin blocks the CYP1A2 enzyme for up to 72 hours after the last dose. Even if you take tizanidine 6 hours later, the enzyme is still shut down. Tizanidine will build up to dangerous levels regardless of timing. The only safe option is to avoid the combination entirely.
What if I’m on a low dose of tizanidine? Is it safer?
No. Even the lowest dose of tizanidine (2 mg) can become toxic when combined with ciprofloxacin. Studies show a 10-fold increase in blood levels-even at low starting doses. There’s no safe threshold when CYP1A2 is blocked. The risk is not dose-dependent in this interaction-it’s all-or-nothing.
Are there any antibiotics that are safe to take with tizanidine?
Yes. Antibiotics that don’t inhibit CYP1A2 are safe alternatives. These include amoxicillin, ampicillin, nitrofurantoin, doxycycline, azithromycin, and cephalexin. For UTIs, nitrofurantoin or amoxicillin are often just as effective as ciprofloxacin and carry no interaction risk with tizanidine. Always ask your doctor for an alternative.
How long should I wait after stopping ciprofloxacin before restarting tizanidine?
Wait at least 5 to 7 days after your last ciprofloxacin dose. Ciprofloxacin stays in your system long enough to keep inhibiting CYP1A2. Even though tizanidine clears quickly (half-life ~2.5 hours), the enzyme takes days to fully recover. Restarting too soon can still cause dangerous buildup. When in doubt, wait a full week.
Can this interaction happen with other antibiotics besides ciprofloxacin?
Yes. Any strong CYP1A2 inhibitor can cause the same problem. This includes fluvoxamine (an antidepressant), enoxacin, and possibly oral contraceptives at high doses. Even some over-the-counter supplements like St. John’s Wort can interfere, though less predictably. Always check with your pharmacist or doctor before starting any new medication while on tizanidine.
Jacob Hepworth-wain
November 19, 2025 AT 16:09Tizanidine and ciprofloxacin together is a recipe for disaster I didn't know about until now
Geethu E
November 20, 2025 AT 07:20As a nurse in Mumbai I've seen this exact scenario three times last year. Patients come in unconscious after mixing these. Doctors don't always check med lists properly. This needs to be screamed from rooftops.
tom charlton
November 20, 2025 AT 16:19This is precisely why clinical pharmacology must be integrated into primary care workflows. The pharmacokinetic interaction between CYP1A2 inhibitors and tizanidine is not merely theoretical-it is empirically validated, clinically significant, and preventable with proper system-level interventions. The fact that this combination persists in prescribing patterns reflects systemic failure, not individual negligence.
anant ram
November 21, 2025 AT 21:26Wow. Just wow. This is terrifying. I had no idea. I'm going to print this out and give it to my doctor. Ciprofloxacin is so common, and tizanidine is so routine for back pain. We need warning stickers on prescriptions. Like, real ones. Like the ones on cigarette packs. This is life-or-death stuff.
Chris Kahanic
November 23, 2025 AT 11:27Interesting read. I've been on tizanidine for years after a spinal injury. My last UTI was treated with amoxicillin. I asked my pharmacist about interactions before filling. Good habit. Always ask.
king tekken 6
November 23, 2025 AT 15:15so like... the government knows this but lets it happen on purpose right? like to keep people docile or something? cipro is everywhere, tizanidine is cheap, and if you pass out from low bp you're not causing trouble. just sayin'
DIVYA YADAV
November 25, 2025 AT 14:09This is why I stopped trusting American medicine. Big Pharma pushes these dangerous combos because they make more money from ER visits and ICU stays. Meanwhile, Indian doctors know better-we use nitrofurantoin for UTIs and avoid cipro unless absolutely necessary. Why? Because we don't let corporate greed override patient safety. The U.S. healthcare system is broken, and this is just one more symptom.
Kim Clapper
November 25, 2025 AT 23:27How can you be so sure this isn't just a scare tactic? I've seen this kind of 'dangerous interaction' rhetoric before-it was later debunked. Are you sure the 43% increase isn't statistically insignificant? Or worse, funded by a competitor to cyclobenzaprine?
Bruce Hennen
November 27, 2025 AT 15:35Incorrect. The FDA contraindication is clear. The Vanderbilt study sample size was 2,107 patients. p-value < 0.001. CYP1A2 inhibition by ciprofloxacin is well-documented in the British Journal of Clinical Pharmacology, 2018. Your skepticism is unfounded and dangerous.
Jake Ruhl
November 27, 2025 AT 20:51okay but what if you're just chill and you take them both at the same time but you're also a yoga master and you meditate for 3 hours before bed? like... maybe your aura blocks the enzyme? i mean, i heard that stress affects liver function so if you're zen you're fine right? i'm just sayin'
Chuckie Parker
November 28, 2025 AT 10:38This is why we need stricter controls on foreign antibiotics. Cipro is overprescribed because it's cheap and imported. American-made alternatives would be safer. We need to ban this combo outright and make doctors take a certification course before prescribing anything that touches CYP1A2.
Evelyn Shaller-Auslander
November 30, 2025 AT 07:02Thank you for this. I'm on tizanidine and just got prescribed cipro. I was about to fill it. Now I'm calling my doctor.
Gus Fosarolli
November 30, 2025 AT 13:54So... cipro is basically the Darth Vader of antibiotics when it comes to tizanidine? I mean, that’s a brutal combo. Like, one’s the muscle relaxant, the other’s the enzyme assassin. No wonder people are dropping like flies. Someone should make a meme: ‘When you take cipro and tizanidine together…’ with a GIF of someone face-planting into a couch.
George Hook
December 1, 2025 AT 00:59I work in a rural pharmacy. We get this combo at least once a month. We call the prescribing doctor every time. Sometimes they’re surprised. Sometimes they’re dismissive. We’ve started printing a one-page handout for patients: ‘Do NOT take ciprofloxacin with tizanidine.’ We hand it to them with the script. It’s small, but it’s something.
jaya sreeraagam
December 1, 2025 AT 13:41I'm a physiotherapist in Chennai and I've had patients come in after fainting because they took cipro for UTI and tizanidine for sciatica. I tell everyone I meet: if you're on muscle relaxants, always ask your doctor about antibiotics. It's not just cipro-fluvoxamine, even some antifungals can do this. Knowledge saves lives. Share this with your family.
Katrina Sofiya
December 2, 2025 AT 20:17This is one of the most important posts I've read this year. Thank you for taking the time to explain this so clearly. I'm sharing it with my entire family. My dad is on tizanidine, and I just found out he was prescribed cipro last month. I'm calling his doctor right now.
kaushik dutta
December 4, 2025 AT 08:30The CYP1A2 enzyme is a critical phase I hepatic metabolizer with a narrow substrate specificity, and its inhibition by fluoroquinolones like ciprofloxacin represents a classic pharmacokinetic drug-drug interaction with high clinical relevance. The 10- to 33-fold increase in tizanidine AUC is not only statistically significant but also pharmacodynamically consequential, leading to exaggerated central nervous system depression and vasodilatory hypotension. This interaction exemplifies the necessity of polypharmacy risk stratification in geriatric and multimorbid populations.
Craig Hartel
December 5, 2025 AT 00:04Man, I'm so glad I found this. My mom had a scary episode last year-collapsed in the kitchen, blood pressure like 70/40. They didn't know why until they found out she'd taken cipro and tizanidine on the same day. She's fine now, but we're all way more careful. If you're on meds, talk to your pharmacist. They know stuff doctors don't have time to remember.