Which Statins Cause the Most Muscle Pain? Real Data on Risk and Alternatives
Statin Muscle Pain Risk Calculator
How Likely Is Muscle Pain with Your Statin?
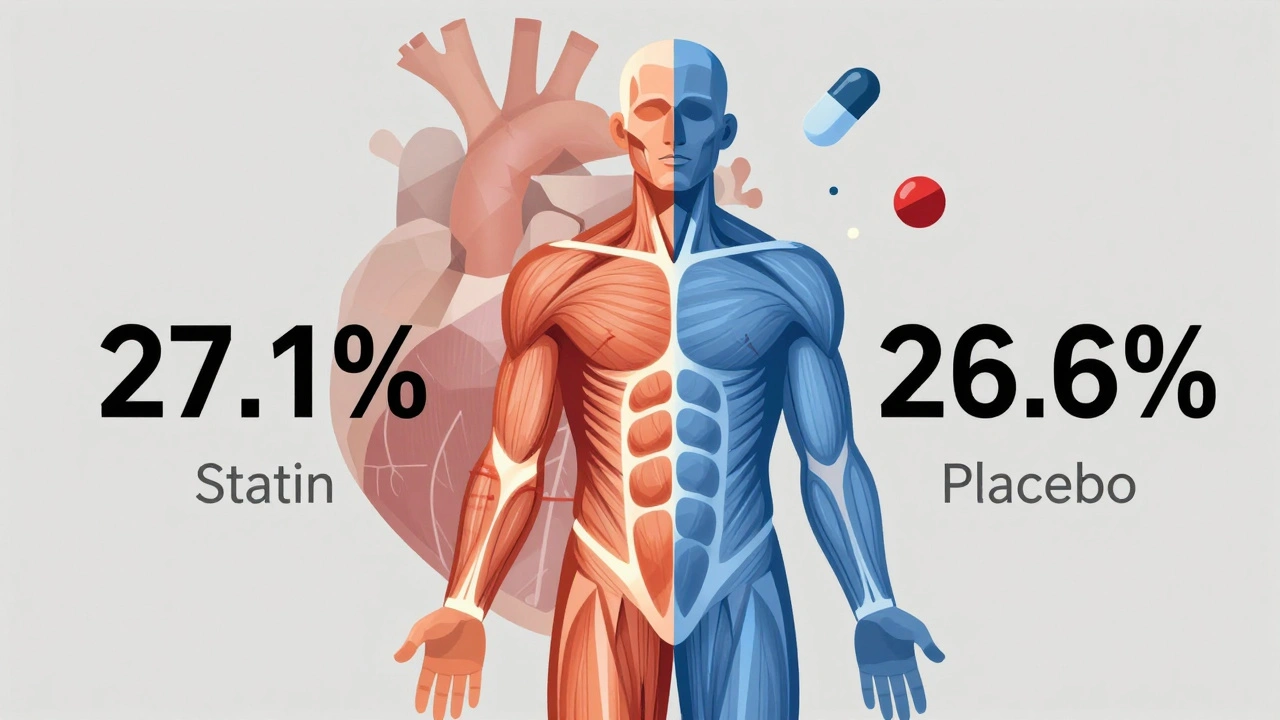
Based on 2022 Oxford study of 123,000+ participants
Estimated muscle pain risk compared to placebo
What to Do If You Experience Muscle Pain
- Don't assume it's the statin—muscle pain is common in older adults
- Try a statin holiday: stop for 2-4 weeks and see if pain resolves
- Switch to a lower-risk statin (pravastatin or fluvastatin often work better)
- Consider lowering your dose
- Check vitamin D and CoQ10 levels
Millions of people take statins to lower their cholesterol and protect their heart. But for many, the fear of muscle pain keeps them from sticking with the medication. You’ve probably heard stories: someone stopped their statin because their legs hurt, or a friend swore the drug made their muscles feel like they’d been run over by a truck. It sounds real. But here’s the twist: statins are likely not the cause in most of those cases.
How Much Muscle Pain Do Statins Actually Cause?
A massive 2022 study from Oxford, tracking over 123,000 people across 23 trials, found something surprising. People taking statins reported muscle pain or weakness in 27.1% of cases. The placebo group? 26.6%. That’s less than a 1% difference. In plain terms, for every 1,000 people taking a statin for a year, only about 11 extra cases of muscle pain were actually linked to the drug. That’s not nothing-but it’s far less than most people think.
Here’s what that means for you: if you start a statin and feel sore, it’s probably not because the drug is wrecking your muscles. More likely, you’re noticing normal aches you’ve always had, or your brain is expecting pain because you heard statins cause it. That’s called the nocebo effect-the opposite of placebo. If you think something will hurt you, your body can make it feel like it does.
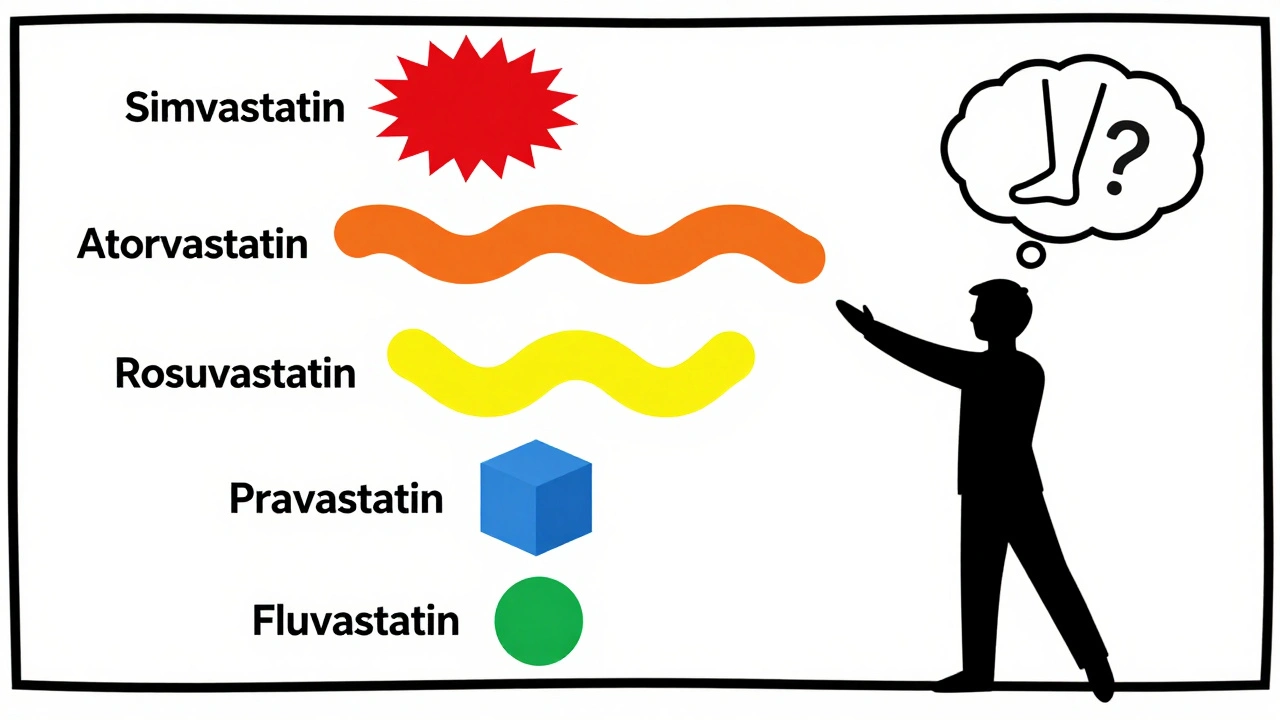
Not All Statins Are Created Equal
Even though statins as a group don’t cause much muscle pain, some are more likely to trigger it than others. The risk isn’t random-it’s tied to how the drug is made and how your body handles it.
Based on clinical data from multiple studies, here’s the ranking from highest to lowest risk of muscle pain:
- Simvastatin - Highest risk. Especially at doses above 40 mg. It’s lipophilic, meaning it easily enters muscle tissue, which may explain why it causes more complaints.
- Atorvastatin - Moderate risk. Popular because it’s strong and lasts a long time, but it’s also one of the most commonly reported for muscle issues.
- Rosuvastatin - Slightly lower risk than atorvastatin. Still potent, but less likely to penetrate muscle cells.
- Pravastatin - Low risk. It’s hydrophilic, so it stays mostly in the liver and doesn’t drift into muscles as easily.
- Fluvastatin - Lowest risk. Used less often, but if muscle pain is your main concern, this is the safest bet.
One study found that people on simvastatin were nearly 80% more likely to report muscle pain than those on pravastatin. Fluvastatin? Only about a third of the risk. That’s a big difference.
Why Does This Happen?
It’s not just about the drug. Your genes matter too. A small group of people-fewer than 3%-carry a gene variant called SLCO1B1. If you have it, your body can’t clear certain statins properly, leading to higher levels in your blood and a greater chance of muscle damage. But even this is rare. Most muscle pain isn’t genetic.
Another factor: drug interactions. Taking statins with certain antibiotics, antifungals, or grapefruit juice can raise statin levels in your blood. That’s when real muscle problems-like rhabdomyolysis-can happen. But that’s extremely rare. The muscle aches most people report? Usually not that.
What Should You Do If You Have Muscle Pain?
If you’re on a statin and feel sore, don’t quit cold turkey. Here’s what works:
- Don’t assume it’s the statin. Muscle pain is common in older adults. Arthritis, vitamin D deficiency, overuse, or even dehydration can cause it.
- Ask for a statin holiday. Stop the drug for 2-4 weeks. If your pain goes away, restart it. If it comes back, it might be the statin. If it doesn’t, you probably had something else going on.
- Try a different statin. If simvastatin was your first choice, switch to pravastatin or fluvastatin. Many people find relief without losing cholesterol control.
- Lower the dose. Sometimes, taking half a pill every day-or every other day-works just as well with fewer side effects.
- Check your vitamin D and CoQ10. Low levels of either are linked to muscle aches. A simple blood test can tell you if you’re deficient.
A Mayo Clinic study found that 68% of people who thought they couldn’t take statins because of muscle pain were able to restart them safely-after learning about the nocebo effect and trying a slow, guided reintroduction.
The Bigger Picture: Benefits vs. Risk
Let’s say you’re 62, have high cholesterol, and a family history of heart disease. Your doctor prescribes a statin. You’re worried about muscle pain. But here’s what you’re really avoiding: a heart attack.
For every 100 people who take a statin for five years, about three major heart events-heart attacks, strokes, or death from heart disease-are prevented. That’s three lives. The number of people who get real, dangerous muscle damage from statins? Less than one in 10,000.
And here’s the kicker: 78% of people who stop statins because of muscle pain do it without talking to their doctor. That’s dangerous. Most of those people could’ve stayed on a safer statin, adjusted their dose, or simply learned that their pain wasn’t caused by the drug.

What If You Really Can’t Tolerate Statins?
Some people truly can’t take any statin-even after switching and lowering doses. That’s called statin intolerance. If that’s you, there are other options:
- Ezetimibe - A pill that blocks cholesterol absorption in the gut. It’s cheap, safe, and works well with or without statins.
- PCSK9 inhibitors - Injectable drugs like evolocumab or alirocumab. They lower LDL dramatically, but cost about $5,850 a year. Insurance often won’t cover them unless you’ve tried everything else.
- Lifestyle changes - Diet, exercise, weight loss, and quitting smoking still matter. They can lower LDL by 20-30% on their own.
But here’s the truth: none of these alternatives match the proven track record of statins. They’re backups, not upgrades.
What’s Changing Now?
The 2022 Oxford study rocked the medical world. The FDA is reviewing statin labels to make them more accurate. The European Medicines Agency already updated its guidelines to say: ‘Muscle symptoms occur just as often with placebo as with statins.’
Doctors are starting to talk differently. Instead of saying, ‘This is a side effect of the drug,’ they’re now saying, ‘Let’s figure out if this is really the statin-or something else.’
And patients? They’re starting to ask better questions. ‘Is this pain from the statin, or from my knees?’ ‘Can I try a different one?’ ‘What’s the real risk?’
Bottom Line
Simvastatin causes the most muscle pain. Atorvastatin comes next. Pravastatin and fluvastatin are your safest bets. But the truth is, for most people, statins aren’t the cause of their muscle pain. The fear is bigger than the risk.
If you’re on a statin and hurting, don’t assume the worst. Talk to your doctor. Try a switch. Get tested. Give yourself a break. You might find your pain disappears without giving up the drug that could save your life.
Clare Fox
December 7, 2025 AT 17:37i’ve been on atorvastatin for 3 years and my knees have always ached. i thought it was the statin. turned out i was just getting old and sitting too much. funny how your brain fills in the blanks, huh?
Arjun Deva
December 9, 2025 AT 04:19THEY’RE LYING!! EVERYTHING IS A CONSPIRACY!! PHARMA IS HIDING THE TRUTH ABOUT STATINS!! THEY’RE NOT JUST CAUSING MUSCLE PAIN-THEY’RE DESTROYING YOUR MITOCHONDRIA, MAN!! THEY’RE TURNING US INTO ZOMBIES SO WE’LL STAY DEPENDENT ON THEIR DRUGS!!
Jackie Petersen
December 9, 2025 AT 15:38so let me get this straight-big pharma’s got us all scared of a drug that barely causes side effects, while they’re pushing expensive injectables that cost more than my car? yeah, right. i’m not falling for it. america deserves better than this nonsense.
Annie Gardiner
December 11, 2025 AT 06:47okay but what if the real problem isn’t the statin… it’s that we’ve been conditioned to believe pain is bad? like, maybe muscle soreness is just our body saying ‘hey, you’re alive’? and we’ve forgotten how to sit with discomfort? i mean, we medicate everything now-sadness, boredom, even quiet.
Rashmi Gupta
December 12, 2025 AT 07:26fluvastatin? really? that’s the safest? i’ve never even heard of it. in india, they just give you simvastatin and tell you to suffer. no one talks about alternatives. we’re treated like numbers, not people.
Kumar Shubhranshu
December 13, 2025 AT 18:06Priya Ranjan
December 15, 2025 AT 02:24people who blame statins for muscle pain are just lazy. if you can’t handle a little discomfort, you shouldn’t be alive. back in my day, we didn’t have fancy blood tests or CoQ10 supplements-we just endured. and we were stronger for it.
Gwyneth Agnes
December 15, 2025 AT 12:18Ashish Vazirani
December 15, 2025 AT 15:34they say 11 extra cases per 1000... but what if you’re one of them? what if your pain is real and no one believes you? i’ve been screaming into the void for years. they call it nocebo. i call it gaslighting.
Kay Jolie
December 15, 2025 AT 18:58the nocebo effect is a fascinating epistemological phenomenon, particularly when contextualized within the biopsychosocial model of pain perception. the pharmacokinetic profile of lipophilic statins-particularly simvastatin-demonstrates enhanced myocellular penetration, which, when coupled with psychosomatic amplification, creates a feedback loop of perceived somatic distress that is statistically indistinguishable from placebo in large cohorts. essentially, your brain is the villain here.
Dan Cole
December 17, 2025 AT 05:26the data is clear, but people don’t want facts-they want validation. the real tragedy isn’t statin side effects-it’s that we’ve turned medicine into a popularity contest where fear sells better than evidence. you don’t need a PhD to understand this, but you do need the courage to face the truth: your pain might be in your head, and that doesn’t make it less real.
Billy Schimmel
December 18, 2025 AT 11:11lol i took simvastatin for two weeks and my legs felt like jelly. i thought it was the drug. turned out i’d been walking my dog 5 miles a day without realizing it. sometimes the body’s just tired, not poisoned.
Shayne Smith
December 19, 2025 AT 10:58my dad switched from atorvastatin to pravastatin and his leg cramps vanished. he didn’t even know there were options. why don’t doctors just tell you this stuff upfront?
Max Manoles
December 20, 2025 AT 21:51great breakdown. i’ve been on fluvastatin for 18 months and have zero issues. i also take vitamin D and avoid grapefruit. simple stuff, but it makes a difference. thanks for the clarity-this is the kind of info that actually helps.