Women vs Men: Why Medication Side Effects Differ by Sex
Medication Side Effect Risk Calculator
This tool estimates your risk of adverse drug reactions based on biological differences between men and women. Women metabolize medications differently due to:
- 40% less liver enzyme CYP3A4 (affects 50% of medications)
- Higher body fat (up to 12% more)
- Slower kidney clearance
- Hormonal fluctuations
Estimated Risk
Women are nearly twice as likely as men to have a bad reaction to the same dose of a medication. It’s not just bad luck. It’s biology, history, and a system built on outdated assumptions. For decades, medical research treated the male body as the default. Women were left out of clinical trials-not because they weren’t important, but because researchers feared pregnancy risks. That decision created a gap that still affects millions today.
Why Women Get More Side Effects
The numbers don’t lie. According to FDA data, women experience adverse drug reactions 80% to 90% more often than men. And it’s not because they take more medicine-though they do. Women use 56% more prescription drugs on average. Even after accounting for usage, they still face higher rates of serious side effects. Why? One major reason is how their bodies process drugs. Women have about 40% less of the liver enzyme CYP3A4 than men. This enzyme breaks down half of all prescription medications, including statins, benzodiazepines, and antidepressants. Slower breakdown means drugs stay in the system longer, increasing the chance of side effects. Body composition plays a big role too. On average, women have 10-12% more body fat than men. Fat-soluble drugs like diazepam (Valium) get stored in fat tissue, which slows their release into the bloodstream. That means the same dose can linger in a woman’s body 20-30% longer than in a man’s. Kidney function also differs. Women clear drugs like lithium and certain antibiotics 20-25% slower than men. That’s not a small difference-it’s enough to push a safe dose into the toxic range. Hormones add another layer. Birth control pills can cut the effectiveness of lamotrigine (a seizure medication) by half. During different phases of the menstrual cycle, metabolism can shift by up to 30%. That means a woman might tolerate a drug fine one week and feel dizzy the next-not because she’s being dramatic, but because her biology changed.Real-World Examples: Drugs That Hit Women Harder
Some medications have clear, documented sex-based risks. Take zolpidem (Ambien). In 2013, the FDA ordered a 50% dose reduction for women after studies showed they metabolized the drug 50% slower. Before that change, women were waking up groggy, even after a full night’s sleep. They were getting into car accidents because the drug hadn’t cleared. After the dose was lowered, adverse event reports from women dropped by 38%. Digoxin, used for heart failure, is another example. At standard doses, women have 20-30% higher blood levels than men. That increases their risk of toxicity by 40%. Many doctors still prescribe the same dose to both sexes. Antidepressants like sertraline and fluoxetine cause nausea and dizziness in women 1.5 to 2 times more often than in men. Women are also 2.3 times more likely to develop dangerous heart rhythm changes (QT prolongation) from antipsychotics like haloperidol. Even common painkillers like ibuprofen and acetaminophen show differences. Women report more stomach upset and liver stress at standard doses. Yet, no sex-specific dosing exists for these drugs.What About Men?
Men aren’t immune to sex-based differences-they just face different ones. They’re 35% more likely to experience sexual side effects from antidepressants and 28% more likely to have trouble urinating from anticholinergic drugs used for overactive bladder or Parkinson’s. They also report fewer side effects overall-not because they’re less sensitive, but because they’re less likely to report them. Studies show men are more likely to ignore symptoms like dizziness or nausea, while women are more likely to seek help. That means the data we have might undercount male side effects, but it doesn’t erase the pattern.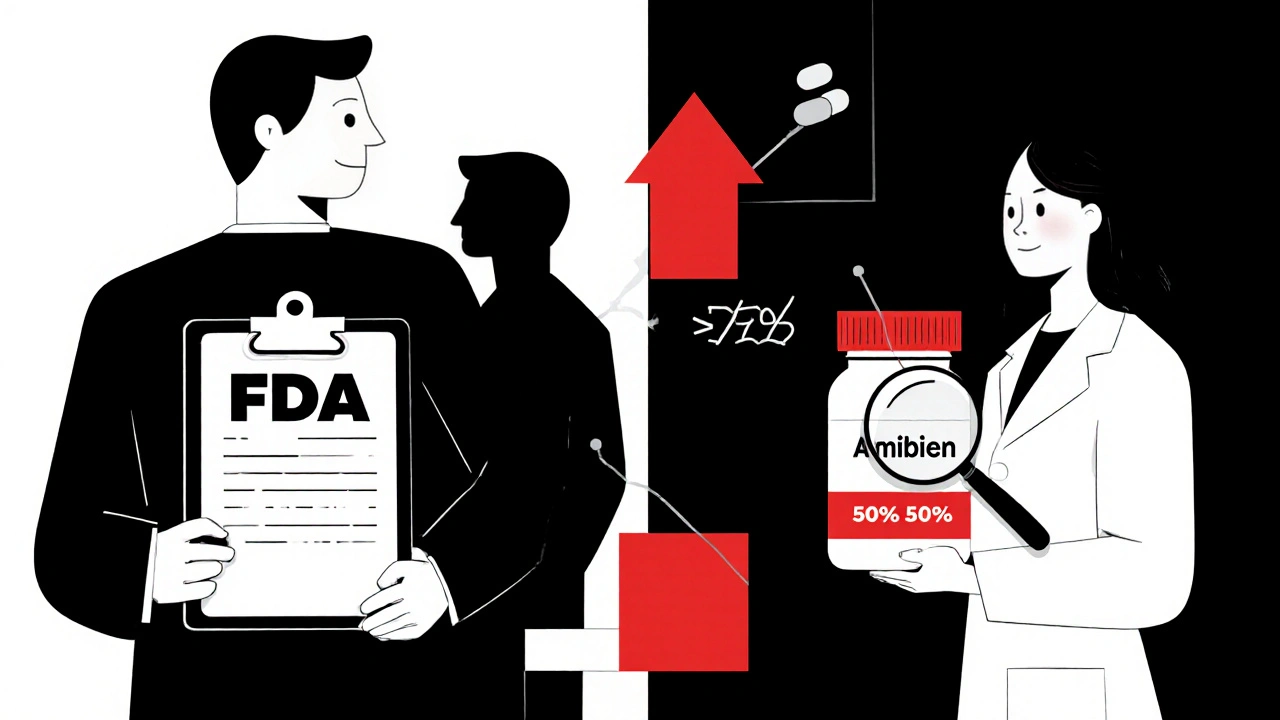
The System That Got Us Here
This isn’t accidental. In the 1970s, the FDA banned women of childbearing age from early clinical trials to protect fetuses. The intent was protective. The result was decades of data based almost entirely on men. Even after the NIH mandated inclusion of women in 1993, progress stalled. Today, women make up nearly half of participants in NIH-funded trials. But only 12% of pharmacokinetic studies-studies that measure how drugs move through the body-analyze results by sex. That means most dosing guidelines still reflect male physiology. Only 15 of the 200 most commonly prescribed medications have sex-specific dosing instructions on their labels. That’s less than 8%. For the rest, doctors guess. Patients guess. And too often, someone pays the price with an ER visit.Doctors Don’t Know What They Don’t Know
A 2022 survey by the American Medical Association found that only 28% of physicians routinely consider sex differences when prescribing. Two-thirds didn’t even know about the FDA’s 2013 zolpidem dose change for women. Medical schools barely teach this. Pharmacology textbooks still treat the human body as male unless otherwise noted. So when a woman says, “This dose makes me sick,” the answer too often is, “It’s fine for most people.” But “most people” isn’t the whole story. And when “most people” are men, women are the ones left behind.
Progress Is Happening-But Too Slow
There’s movement. The European Medicines Agency now requires sex-stratified data in all Phase III trials. The FDA launched its “Sex and Gender Roadmap” in 2023, aiming to make sex-based analysis standard by 2026. The NIH invested $12.5 million in a new research center focused on sex differences in medicine. A University of California study called JUST Dose is using AI to build personalized dosing models based on sex, weight, age, and metabolism. Early results show a 40% drop in adverse events when sex-specific doses are used. Companies like Adyn and Womb Society are building drugs specifically for women’s biology. And investors are taking notice-$1.4 billion flowed into femtech in 2023. But these efforts are still tiny. Less than 0.5% of pharmaceutical R&D is focused on sex-specific drugs. And without mandatory rules, progress will keep crawling.What You Can Do
If you’re a woman taking medication:- Ask your doctor: “Was this dose tested on women?”
- Check the FDA’s Drug Trials Snapshots for sex-disaggregated data on newer drugs.
- Keep a side effect journal-note timing, severity, and menstrual cycle phase.
- If you’re experiencing side effects others don’t, don’t assume you’re overreacting. You might just need a lower dose.
- Start asking: “Is this dose appropriate for a woman?”
- Use the FDA’s Sex and Gender Roadmap as a reference.
- Consider body weight, fat percentage, and hormonal status-not just age and kidney function.
The Bigger Picture
This isn’t just about fairness. It’s about cost. Adverse drug reactions cost the U.S. healthcare system $30 billion a year. Women account for 63-70% of those severe reactions. Fixing this isn’t a women’s issue-it’s a public health issue. We don’t need separate drugs for men and women. We need better science. We need dosing that reflects real biology, not historical convenience. We need labels that tell the truth. The tools exist. The data is there. What’s missing is the will to use it.The next time you hear someone say, “It’s the same for everyone,” remember: biology doesn’t work that way. And neither should medicine.
Why do women have more side effects from medications than men?
Women have different body composition, hormone levels, and enzyme activity than men. They typically have 40% less CYP3A4 liver enzyme, which slows the breakdown of many drugs. They also have higher body fat, which affects how fat-soluble medications are stored and released. Kidney clearance is slower, and hormonal changes during the menstrual cycle can alter drug metabolism by up to 30%. These biological differences mean the same dose can have stronger or longer-lasting effects in women.
Is the zolpidem (Ambien) dose different for women?
Yes. In 2013, the FDA reduced the recommended starting dose of zolpidem for women by 50% because studies showed women metabolize the drug 50% slower than men. This led to next-day drowsiness, impaired driving, and accidents. After the change, adverse event reports from women dropped by 38%. This remains one of the few clear examples of sex-specific dosing in U.S. drug labeling.
Are men’s medication side effects ignored too?
Not ignored-but underreported. Men are more likely to experience sexual side effects from antidepressants and urinary retention from anticholinergics. But they’re also less likely to report symptoms or seek help. This creates a reporting gap that makes it seem like side effects affect women more. In reality, men face different risks that are often overlooked because research and labeling focus on female-specific outcomes.
Why don’t drug labels have sex-specific dosing?
Because most drugs were tested primarily on men, and regulatory agencies didn’t require sex-based analysis until recently. Even now, only 15 of the 200 most commonly prescribed medications include sex-specific dosing instructions. Updating labels takes years, and many manufacturers don’t prioritize it unless forced by regulation. The FDA only began requiring sex-disaggregated data in new trials in 2018, and compliance is still inconsistent.
What’s being done to fix this problem?
The FDA’s 2023 Sex and Gender Roadmap aims to make sex-based analysis standard across all drug approvals by 2026. The NIH is funding new research centers focused on biological differences. Some countries, like those in the EU, now require sex-stratified data in clinical trials. Companies are also investing in femtech and sex-specific drug development. But progress is slow-only 32% of cardiovascular drug trials currently analyze results by sex, and most doctors still aren’t trained to consider these differences.
Can I ask my doctor for a lower dose if I’m a woman?
Absolutely. If you’re experiencing side effects that men on the same drug don’t report, ask if a lower dose might work for you. Start with a conversation: “I’ve read that women sometimes need lower doses of this medication. Can we try reducing it?” Many drugs can be safely adjusted. Don’t assume the prescribed dose is perfect for your body-it was likely designed for the average male patient.
Conor McNamara
November 19, 2025 AT 03:47Leilani O'Neill
November 19, 2025 AT 04:15Riohlo (Or Rio) Marie
November 20, 2025 AT 13:40steffi walsh
November 22, 2025 AT 10:24Heidi R
November 23, 2025 AT 07:09Brenda Kuter
November 25, 2025 AT 05:55Shaun Barratt
November 25, 2025 AT 21:10Iska Ede
November 25, 2025 AT 21:23Gabriella Jayne Bosticco
November 26, 2025 AT 23:31Sarah Frey
November 28, 2025 AT 07:29Katelyn Sykes
November 29, 2025 AT 02:40Gabe Solack
December 1, 2025 AT 01:19