Self-Advocacy Tips for Meniere's Disease Patients
Meniere's Disease Self-Advocacy Checklist Tracker
Your Self-Advocacy Checklist
Living with Meniere's disease is a chronic inner‑ear disorder that can feel like a roller‑coaster-spells of vertigo, ringing ears, and fluctuating hearing that turn everyday life into a guessing game. When doctors prescribe meds, diet tweaks, or even surgery, the real challenge often begins: making sure the care you receive matches your needs, preferences, and lifestyle. That’s where Meniere's disease advocacy comes in. Below you’ll find a step‑by‑step guide to taking charge of appointments, treatment choices, and long‑term wellness without feeling lost or powerless.
1. Get Clear on What You’re Dealing With
Before you can argue for the right care, you need a solid mental model of the disease. Vertigo is the sensation that the room is spinning, often lasting minutes to hours and triggered by head movements. Tinnitus is the persistent ringing, buzzing, or hissing that many patients hear even in a quiet room. Hearing loss usually starts low‑frequency and can become permanent if the disease progresses. Finally, Aural fullness feels like pressure or a clogged ear.
Knowing these four hallmark symptoms helps you recognize what’s normal disease fluctuation and what might signal a complication that needs a different approach.
2. Map Out Your Care Team
Advocacy starts with knowing who does what. Here are the key players:
- Otolaryngologist (ENT) - specializes in ear, nose, and throat disorders, can confirm diagnosis and discuss surgical options.
- Audiologist - performs hearing tests, fits hearing aids, and tracks changes over time.
- Primary care physician - coordinates overall health, monitors comorbidities like hypertension that affect inner‑ear fluid balance.
- Vestibular rehabilitation therapist - teaches balance exercises that reduce fall risk during vertigo attacks.
- Support group facilitator - provides peer‑to‑peer emotional support and practical tips.
When you know each professional’s scope, you can ask targeted questions and avoid redundant tests.
3. Prepare a One‑Page Health Summary
Doctors appreciate concise, data‑driven info. Create a one‑page document that includes:
- Diagnosis date and confirming test results (e.g., electrocochleography, MRI).
- Frequency, duration, and triggers of vertigo episodes.
- Current meds, dosages, and side‑effects.
- Recent hearing thresholds from your audiologist.
- Allergy list and other chronic conditions.
Print a copy for every appointment and keep a digital version you can email if asked for records. This small act saves time and shows you’re serious about your care.
4. Master the Art of Question‑Asking
Most patients feel intimidated, but a prepared list can turn the conversation into a collaborative problem‑solving session. Examples:
- "What evidence supports this medication for my vertigo frequency?"
- "If I choose a low‑salt diet, how much should I reduce my sodium intake each day?"
- "Are there non‑surgical options that could preserve my hearing longer?"
- "What are the warning signs that I need to seek urgent care?"
Notice how each question asks for specifics, not vague reassurance.

5. Document Every Decision
After each visit, write a short recap: what was discussed, what you agreed to try, and any follow‑up dates. A simple table works well:
| Date | Provider | Decision | Next Step |
|---|---|---|---|
| 09/02/2025 | Otolaryngologist | Start low‑dose diuretic | Revisit in 4 weeks |
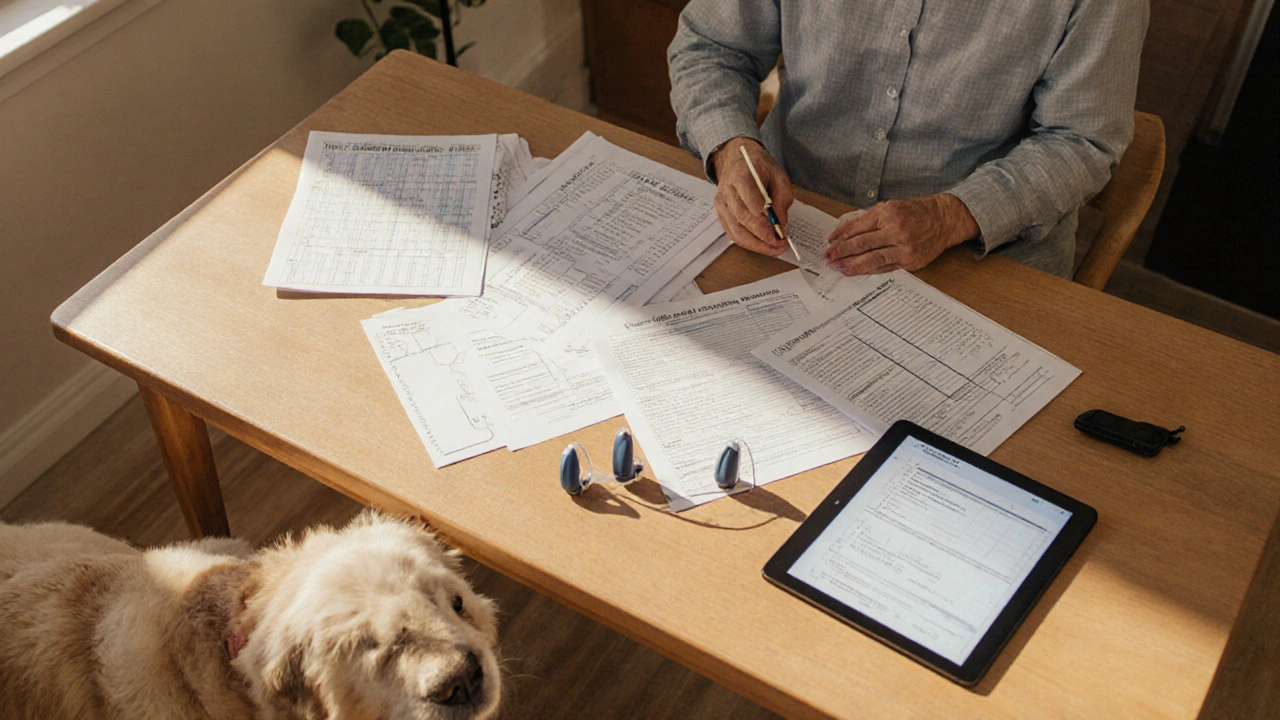
| 09/10/2025 | Audiologist | Fit behind‑the‑ear hearing aid | Adjust gain after 2 weeks |
Having a written trail makes it harder for anyone to overlook a recommendation and gives you leverage when you need to revisit a choice.
6. Use Advocacy Tools to Bridge Gaps
Sometimes a simple tool can turn a passive patient into an active partner. Below is a quick comparison of the most useful resources.
| Tool | What It Does | How to Implement |
|---|---|---|
| Patient portal messaging | Allows you to ask follow‑up questions without waiting for the next visit. | Enroll through your clinic’s online portal; keep messages concise. |
| Symptom diary app | Tracks vertigo intensity, diet, and medication timing. | Log entries daily; share PDF with your ENT before appointments. |
| Second‑opinion service | Provides an independent review of imaging and treatment plans. | Submit copies of your records; schedule a virtual consult within 2 weeks. |
| Patient advocacy organization | Offers legal advice, insurance navigation, and peer mentoring. | Join the Meniere’s Disease Foundation; attend quarterly webinars. |
7. Harness Peer Support
Living with unpredictable attacks can feel isolating. A Support group connects you with people who speak the same language of dizziness and hearing change. In my experience, the best groups have two features:
- Monthly virtual meetings led by a certified audiologist-so you get professional input alongside personal stories.
- A private forum where members share diet logs, medication side‑effects, and coping tricks.
When you hear that someone else successfully managed a trigger (like caffeine), you gain a concrete tactic rather than vague encouragement.
8. Know Your Rights
Patient rights are not abstract; they translate into everyday actions:
- Right to information - You can ask for plain‑language summaries of test results.
- Right to a second opinion - Insurers must cover a reasonable second‑opinion consult for major procedures.
- Right to accessible records - Under HIPAA, you can request electronic copies of all your ear‑related imaging within 30 days.
When you invoke a right, you’re not being confrontational-you’re simply ensuring the system works as intended.
9. Quick-Reference Self‑Advocacy Checklist
- Update your one‑page health summary before every appointment.
- Bring a symptom diary that covers the last two weeks.
- Ask at least two specific questions about any new recommendation.
- Record the provider’s name, specialty, and next steps in the action log.
- Schedule a follow‑up call within 48‑72hours if you haven’t heard back from the clinic.
- Join a reputable Meniere’s support community for peer tips.
- Review your insurance policy for coverage of second‑opinion visits.
Cross‑checking this list each month keeps you on top of your health and shows providers you’re an engaged partner.

Frequently Asked Questions
How often should I see my otolaryngologist?
If your vertigo attacks are stable and you’re on a medication regimen, a six‑month follow‑up is typical. However, any change in frequency, intensity, or new hearing loss warrants an earlier visit.
Can a low‑salt diet really reduce attacks?
Studies show that reducing sodium to under 1500mg per day can lower inner‑ear fluid pressure, which often translates into fewer and milder vertigo spells. Consistency is key-sporadic changes won’t move the needle.
What should I do if a medication makes my tinnitus worse?
Document the timing and intensity of the tinnitus surge, then call your prescribing doctor. Ask whether a dose adjustment or a different class of drug (e.g., from a loop diuretic to a thiazide) might help.
Is surgery ever necessary for Meniere’s disease?
Surgery is considered when attacks are frequent (more than three per month) and medications plus lifestyle changes have failed. Options include endolymphatic sac decompression or vestibular nerve section; each carries different hearing‑preservation risks, so a second opinion is strongly advised.
How can I talk to my insurer about coverage for vestibular rehab?
Request a written recommendation from your ENT that lists vestibular rehabilitation as medically necessary. Submit it with a prior‑authorization request, citing CPT code 92540. If denied, appeal using the denial letter as evidence of clinical need.
Arjun Santhosh
September 30, 2025 AT 13:18Thanks for the checklist, will try it out.
Stephanie Jones
September 30, 2025 AT 14:41Reading through the self‑advocacy steps feels like navigating a maze of medical jargon, yet the underlying message is clear: we must become our own champions in a system that often forgets the human behind the symptoms.
Nathan Hamer
September 30, 2025 AT 17:28Wow, this guide is a treasure trove! 😃 First off, the one‑page health summary idea is pure gold – having a concise snapshot saves everyone from repetitive explanations. 🚀
Second, the symptom diary app recommendation cannot be overstated; logging vertigo intensity, diet, and medication timing gives your ENT data you can’t fake. 📊
Third, the emphasis on asking specific questions turns a passive appointment into a collaborative problem‑solving session – I always jot down at least two bullet points before I sit down.
Fourth, the advocacy tools table is a brilliant visual aid; patient portal messaging, second‑opinion services, and insurance navigation are all essential pieces of the puzzle.
Fifth, the checklist itself is perfectly designed – checking boxes and watching the progress bar gives a dopamine hit that motivates consistency.
Sixth, the support‑group tip about monthly audiologist‑led virtual meetings adds professional oversight to peer support, which is rare.
Seventh, the rights section reminds us that HIPAA isn’t just legalese; it’s a lever we can pull to get records promptly.
Eighth, the mention of low‑salt diet under 1500 mg sodium truly makes a difference – I’ve seen my attacks shrink after cutting out processed foods.
Ninth, the follow‑up call within 48‑72 hours rule ensures we don’t fall through the cracks of busy clinics.
Tenth, the insurance second‑opinion coverage note can save thousands when surgery looms.
Eleventh, the table of “advocacy tools vs. standard care” is a quick reference I’ll bookmark.
Twelfth, the FAQ section neatly addresses common concerns – perfect for newcomers.
Thirteenth, the actionable checklist items are simple enough to implement right away.
Fourteenth, the emphasis on documenting every decision creates a paper trail that protects us.
Fifteenth, the overall tone is empowering without being preachy – exactly what patients need.
All in all, this is a masterclass in self‑advocacy for Meniere’s disease. 🙌
Tom Smith
September 30, 2025 AT 19:41Nice breakdown, but remember not every patient has the time to fill out a spreadsheet after each visit – realism matters.
Kyah Chan
September 30, 2025 AT 21:21While the enthusiasm is commendable, the suggestion to engage in weekly virtual audiology sessions may be impractical for those in remote regions lacking stable internet connectivity.
Ira Andani Agustianingrum
October 1, 2025 AT 00:41Hey there, I completely agree that keeping a simple symptom diary on your phone can make a huge difference. I’ve found that a quick note after each vertigo episode – what I ate, how long it lasted, and whether I felt any ringing – helps my doctor spot patterns fast. Also, updating the one‑page health summary right before the appointment saves us both from re‑explaining the basics. Give it a try and let us know how it works for you!
James Higdon
October 1, 2025 AT 01:48While your casual approach is helpful, it’s essential to stress that patient rights are not merely suggestions; they are enforceable under HIPAA and ACA regulations.
Wanda Smith
October 1, 2025 AT 04:18One could argue that the entire medical establishment is built on a framework of controlled narratives, designed to keep patients dependent on proprietary protocols.
Bridget Jonesberg
October 1, 2025 AT 05:41The notion that we merely "join a support group" overlooks the sociocultural dynamics that shape patient experiences; however, the curated list of vetted communities does provide a structured avenue for collective knowledge exchange, which in turn mitigates the epistemic isolation often felt by those navigating chronic vestibular disorders.
Marvin Powers
October 1, 2025 AT 07:38Interesting take, but let’s not forget that community wisdom can sometimes clash with evidence‑based practices – a balanced perspective is key, and sharing personal anecdotes alongside peer‑reviewed research creates a richer tapestry of understanding for all of us.
Christopher Montenegro
October 1, 2025 AT 10:41The checklist, while thorough, suffers from an overreliance on patient‑generated data, which can introduce variability and bias into clinical decision‑making processes; clinicians must therefore calibrate such inputs against standardized metrics to avoid diagnostic drift.
Kyle Olsen
October 1, 2025 AT 12:04Indeed, the reliance on self‑reported diaries is a methodological flaw; still, the practicality of having a tangible record cannot be dismissed outright – it serves as a bridge between patient experience and provider analysis, albeit a bridge that must be reinforced with objective testing.
Sarah Kherbouche
October 1, 2025 AT 14:18It is crucial that we highlight the patriotic duty of demanding full coverage for vestibular rehab – the government should not shirk its responsibility to its citizens.
MANAS MISHRA
October 1, 2025 AT 15:08Absolutely, securing coverage is a right, and filing a proper prior‑authorization with the CPT code 92540 can often expedite the process – remember to attach a physician’s letter of medical necessity.
Lawrence Bergfeld
October 1, 2025 AT 17:38Guys, keep it short: update your health summary, bring a diary, ask two questions – repeat each visit.
Chelsea Kerr
October 1, 2025 AT 18:44👍 Great summary! Adding a quick note on medication side‑effects in your diary can alert your ENT to subtle changes before they become big problems. 😊
Tom Becker
October 1, 2025 AT 21:31Did you ever consider that the push for patient‑portal messaging is a surveillance tactic, feeding data straight to big pharma analytics?
Laura Sanders
October 1, 2025 AT 22:54While conspiracies are entertaining, the reality is that patient portals improve communication efficiency – a balanced view is more constructive.
Zara @WSLab
October 2, 2025 AT 01:08Love the practical tips! 🤗 Could someone share a favorite symptom‑tracking app? I’m looking for something user‑friendly.
Kyle Rensmeyer
October 2, 2025 AT 02:48Sure, but remember that most apps are funded by entities that want your data – always read the privacy policy.